Sopris Health has recently announced the launch of the latest version of their AI-driven, mobile clinical documentation system. The tool, Sopris Assistant, assists physicians in composing clinical notes and imports them into an EHR system in 45 seconds or less, as per Sopris.
This past May, the Denver-based startup released a similar app-based technology that utilized a wearable device and AI to listen in on patient-provider interactions to capture and document relevant information for clinical notes. Patrick Leonard, cofounder and CEO of Sopris Health, explained the new system to be a huge improvement in the efforts of automating clinical documentation.
“We served tens of thousands of visits with our customers and have worked with several large institutions — we were in the Cedars-Sinai tech accelerator last fall, so we spent a lot of time basically living in Cedars-Sinai in Los Angeles, working with physicians and people there to really get a deep understanding of how they do documentation,” Leonard explained in a demonstration of the platform for MobiHealthNews.
READ MORE: Cedars-Sinai Using Alexa in Smart Hospital Room Pilot Program
The Sopris Assistant app is now available on iOS to U.S. health care providers and has been shown to reduce time spent on documentation processes more than alternative solutions. The app not only speeds up the process of clinical note input but allows the physician to devote more time to more urgent responsibilities as well. The latter is an attribute of the system Sopris believes will minimize physician burnout and cognitive load.
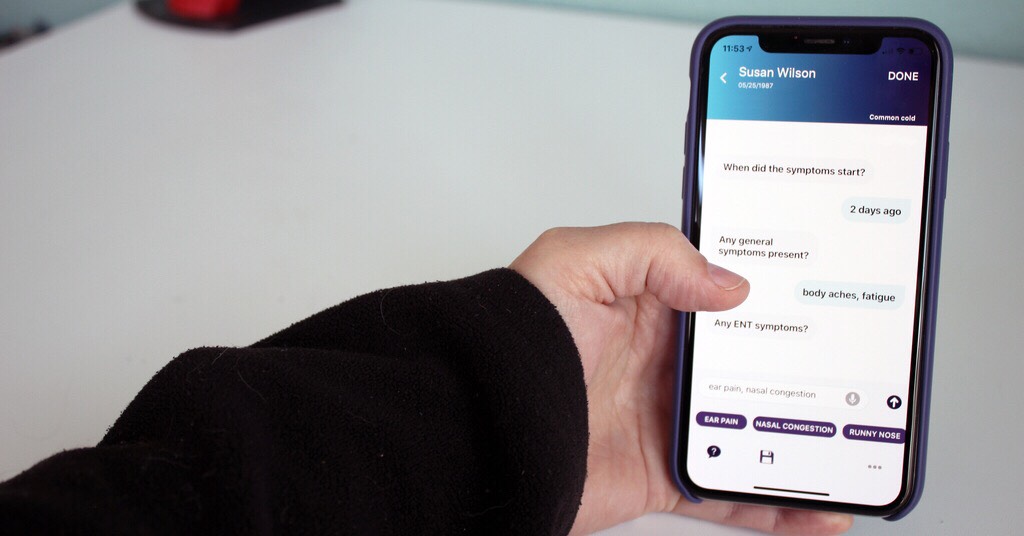
“Throughout our onsite clinic experience with providers, we’ve observed a variety of scenarios in a variety of specialties where practitioners chose to keep technology out of the room or chose to leave part of the clinic note out of the patient conversation,” said Leonard. “If scribes need to ask a handful of questions after physicians see a patient, so will a technology. The Sopris Assistant is trained to know what questions to ask by specialty, by visit type, by note type in the simplest exchange possible.”
READ MORE: Michigan Researchers use 3D Printing to Aid Arthritis Patients at Low Costs
Medical providers use a face or touch ID to authorize the opening of the app, then tap a selected patient from a list of imported EHR data. The Sopris Assistant walks the provider through an interactive text-like chat interface, asking for the type of visit, a few questions answered via voice, and then for a final review of the generated note before submission.
The team behind the technology worked extensively with a clinical advisory board to train the virtual assistant to know what to ask the physician as well as how to complete documentation. Sopris aimed to generate a product that gave real-time and fully automated medical documentation that is more than mere conversational data.
The company studied tens of thousands of physician notes on their previous listening-AI platform to find that in all notes studied, humans were needed to go back and add content to the notes after examination. This led them to the realization that simply recording the conversations between patient and provider did not yield enough relevant data to compose the note.
“It’s not uncommon for us to hear from a prospective customer at 10 p.m. after another evening of missed personal priorities in the name of pajama time,” said Leonard, referring to physicians who must often devote too much time to clinical notetaking. “We know providers are desperate for a solution that mitigates today’s demands, immediately providing real value, real time savings. Their need is palpable and we push ourselves to onboard them within days.”
Through AI text chats, Sopris Health’s new app saves time on clinical documentation https://t.co/i7UedscILV #digitalhealth pic.twitter.com/Qld0UNH7oN
— Berci Meskó, MD, PhD (@Berci) March 20, 2019
READ MORE: FDA Cleared AI Systems for Diagnosing Breast Cancer and Brain Bleeding
Sources: MobiHealthNews, VentureBeat






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.