ASH 2023: Focus on Myelofibrosis
Advertisement
A noninvasive magnetic resonance imaging technique can effectively evaluate bone marrow in patients with myelofibrosis.
CALR-1 mutation is an important risk factor for both drug survival and longevity in momelotinib-treated patients with MF.
A significant proportion of patients with myelofibrosis undergoing HSCT experience poor graft function.
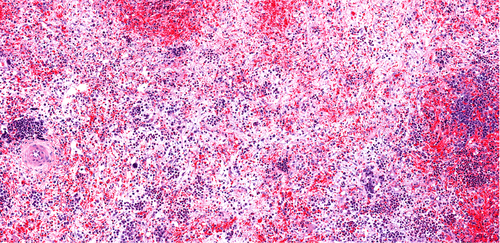
Transfusion independence response was linked to bone marrow reticulin fibrosis improvement in patients with myelofibrosis.
A study found that JAK2 V617F mutations were associated with improved OS and PFS after HCT in patients with myelofibrosis.
The Reticulin, Collagen, Osteosclerosis score is clinically and prognostically relevant in secondary myelofibrosis.
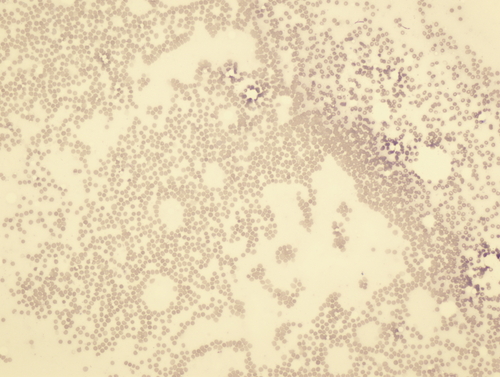
Changes in bone marrow microbiome and proteome can help distinguish between patients with ET and those with prefibrotic PMF.
Patients with relapsed or refractory MF treated with TP-3654 monotherapy showed promising early outcomes.
A study compared health-related QOL and symptom burden in patients with prefibrotic MF and those with overt MF.
More than half of patients with low-risk myelofibrosis have evidence of disease progression.
The risk of CV-related mortality risk in patients with primary MF has not increased following the approval of ruxolitinib.
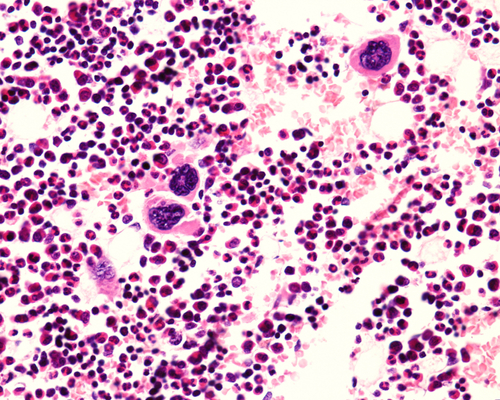
Megakaryocytes derived PF4 play an important role in the progression of myelofibrosis.
Serial sensitive molecular monitoring of JAK2 at defined points is a viable predictive marker for relapsed myelofibrosis.
In vivo T-cell depletion with antithymocyte/antilymphocyte globulin prior to HSCT is effective at reducing GVHD.
Treating myelofibrosis patients with ruxolitinib before, during, and after HSCT is safe and effective.
Persistence of cells with MF-associated driver mutations following allogeneic HSCT was linked to outcomes.
Ropeginterferon alfa-2b is an effective treatment for patients with primary myelofibrosis in the pre-/early fibrotic stage.
Hemoglobin and platelets are associated with overall survival in patients with myelofibrosis following allogeneic HSCT.
Treatment-naïve myelofibrosis patients who received navitoclax plus ruxolitinib saw a significant reduction in spleen ...
Advertisement














 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.