
Stent placement is a common procedure in the United States; in 2004, over a million coronary stent procedures took place. Stents, small tubes that open the artery, are often placed during or right after angioplasty, a procedure performed to allow blood to flow through narrow or blocked blood vessels. The goal of using a stent is to keep the artery open overtime. Typically, stents are made of a metal mesh material, but they are sometimes made of fabric; these are more common when treating larger arteries.
As with any procedure, patients receiving a stent will likely wonder what to expect afterward.
Recovery and Return to Normal Activities
Patients who undergo non-emergency treatment will likely stay in the hospital overnight to be monitored. They may be able to return to light, routine activities during the first few days after the procedure. Bruising or discoloration may occur at the catheter insertion site, as well as soreness when pressure is applied, and patients can expect to feel more tired than usual for a few days. Patients should drink plenty of fluids to help flush out any contrast dye.
About a week after the procedure, the doctor may say it’s okay to return to more moderate activities, and work, but avoid any activities that cause shortness of breath or chest pain. About three to four weeks after the procedure, it may be safe to resume strenuous physical activity and lifting heavy objects; patients must receive clearance from their doctor.
For some patients, their doctor may also recommend lifestyle changes. This could include exercise, quitting smoking, and following a healthy diet.
Patients who undergo stent placement following a heart attack may have a different recovery. Their hospital length of stay and return to activities will likely be longer.
During the recovery period, patients should seek medical attention if they experience any of the following:
- Bleeding, swelling, pain, or discomfort at the catheter insertion site
- Redness, swelling, drainage, or fever indicative of infection
- Changes in temperature or color in arm or leg where the procedure was performed
- Faintness or weakness
- Chest pain
- Shortness of breath
Patients may be encouraged to attend at least one follow-up appointment to make sure the catheter insertion site is healing properly. A stress test may also be performed several weeks after the procedure, which will help the doctor determine appropriate activity and exercise recommendations.
Depending on the stent used, patients may have to be monitored to ensure the stent is working properly and is in the right place. Airway stents may be checked through bronchoscopy several weeks after the procedure; a chest X-ray or CT scan could also be used. A CT angiograph or ultrasound may be performed to check a stent graft is not leaking several weeks following placement, and possibly for the long-term. If leaking or another issue occurs, the stent may need to be continuously monitored, and if the leak is severe, surgical intervention may be necessary.
Medications to Take
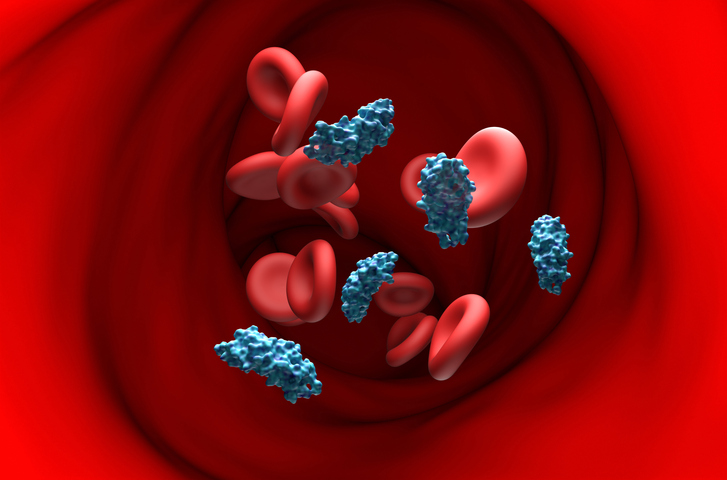
After the procedure, it is important to adhere to the doctor’s recommended treatment because this could help prevent blood clots that may re-block the artery. One way to prevent this is through antiplatelet medication, including aspirin and a P2Y12 inhibitor. Which P2Y12 inhibitor a patient is prescribed—clopidogrel, prasugrel, or ticagrelor—is individualized for each patient. Some patients will undergo dual antiplatelet therapy (DAPT), a combination of aspirin and a P2Y12 inhibitor. Treatment duration will depend on a patient’s cardiac history, their bleeding risk, and whether they received a drug-eluting stent (DES) or a bare metal stent (BMS).
Possible Complications, Stent Failures
As DocWire News previously reported, possible risks associated with angioplasty and stent placement include:
- Bleeding or infection at the catheter insertion site
- Blood clot/blood vessel damage
- Abnormal heart rhythms such as Atrial Fibrillation
- Heart attack
- Stroke
- Chest pain/discomfort
- Rupture or closing of the coronary artery
- Allergic reaction to/kidney damage from contrast dye
Blood clots are significantly more likely to occur if patients do not continue taking their prescribed blood thinners after the procedure. Blood clots could result in serious, sometimes fatal, outcomes, including heart attack, stroke, or venous thromboembolism.
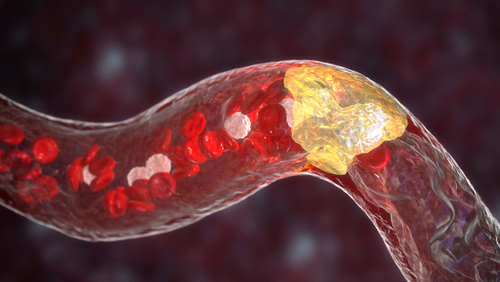
Chest pain should be taken seriously as it could indicate that the artery has become re-blocked, a condition known as restenosis. Restenosis can be treated in a number of ways:
- Re-stenting/re-expanding the stent
- Supplementary medications
- Lifestyle changes to control coronary artery disease
For some patients, surgery may be necessary. Coronary artery bypass graft surgery (CABG) is an option in this case. CABG is performed by taking a healthy blood vessel from somewhere else in the patient’s body and using it to bypass the blocked artery by attaching one end of it above the blocked area and the other end below it, allowing blood to flow freely through the newly placed vessel.
Does Stent Type Matter?
Evidence does not suggest significant differences in outcomes whether patients receive DES or BMS. A 2016 study published in the New England Journal of Medicine assessed the composite outcome of death from any cause and nonfatal spontaneous myocardial infarction based on stent type. The researchers found similar between-group outcomes: “At 6 years, the rates of the primary outcome were 16.6% in the group receiving drug-eluting stents and 17.1% in the group receiving bare-metal stents (hazard ratio, 0.98; 95% confidence interval [CI], 0.88 to 1.09; P=0.66). There were no significant between-group differences in the components of the primary outcome.”
Similarly, a study published in JAMA Internal Medicine compared outcomes for patients who received DES versus BMS. Data were gathered from the Duke Databank for Cardiovascular Disease on patients undergoing their initial revascularization between Jan. 1, 2000, and July 31, 2005, who received either DES (n = 1,501) or DES (n = 3,165). After 24 months, DES patients had lower rates of target vessel revascularization after 24 months, but there were no significant between-group differences in death or myocardial infarction.
Sources: American Heart Association; National Heart, Lung, and Blood Institute; Mayo Clinic; The Society of Cardiovascular Angiography and Interventions; Cleveland Clinic





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.