
Acute kidney injury (AKI) is common, affecting nearly one-fifth of all hospitalized patients and two-thirds of critically ill patients. In an insightful report in Kidney360 in 2023, Erin Barreto, PharmD, PhD, and colleagues from the AKINow Recovery workgroup1 cite some of the key gaps in care that seem commonplace and preventable in managing AKI, including issues of transition of care, patient education, collaborative care delivery, inconsistent evaluation of kidney health after discharge, and lack of best practices in selecting post-AKI medications.
In their report, the authors concluded that “proactive attention to developing, testing, and implementing evidence-based practices in the identified areas is needed to improve the health outcomes of AKI survivors, the care quality they receive, and the healthcare experience encountered by themselves, their loved ones, and their clinician team.”
Following this report, a more recent concept called dialytrauma has emerged. Originally, dialytrauma referred to harmful adverse events associated with continuous renal replacement therapy or dialysis. The recent publication in the Journal of the American Society of Nephrology titled “ASN Kidney Health Guidance on the Outpatient Management With Dialysis-Requiring Acute Kidney Injury”2 has broadened the term to include the potentially harmful effects of dialysis in patients with AKI who transition from an inpatient to an outpatient setting.
Preventing dialytrauma is a priority for the approximately 12,000 patients with AKI requiring dialysis (AKI-D) who transition from inpatient to outpatient settings in the United States. At least in some proportion of these patients, preventing dialytrauma might allow their kidneys to recover and for them to discontinue dialysis.
In the American Society of Nephrology (ASN) guidance, Anitha Vijayan, MD, and colleagues2 offer several sensible recommendations, albeit some based more on common sense and opinion than strong evidence. These are summarized in the Table.
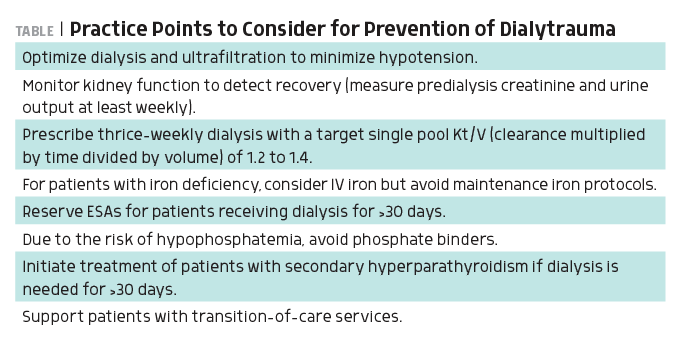
The ASN guidance correctly emphasizes the overarching importance of minimizing intradialytic hypotension (IDH). (The review on IDH by Andrew Davenport, MD, MB BChir, is worth reading.3) Preventing IDH begins with knowing the patient. In terms of transition of care from an inpatient to an outpatient setting, the emphasis on a warm handoff is on point. A warm handoff needs to be rich in terms of information and advice provided to the receiving dialysis team from their inpatient colleagues about how to manage the patient.
During the handoff, specific questions about how to prevent IDH are critical. Has the patient’s dry weight been established? How well has the patient tolerated volume removal while undergoing dialysis? Is there underlying cardiac pathophysiology at play (eg, diastolic dysfunction)? Has the prescription been customized (eg, cooling the dialysate, using albumin, using a sequential strategy [an initial period of hypotension followed by solute clearance during dialysis])? Patients can be susceptible to IDH for a variety of reasons including incorrect estimation of dry weight, diastolic dysfunction, presence of anemia, slow recovery from the vasoactive effects of sepsis syndrome, hypoalbuminemia, and so on.
Another point covered by the ASN guidance is the issue of monitoring the patient for recovering kidney function. Sometimes it’s simply an issue of asking the patient whether they have started passing urine, and if so, how much. Then it is worth measuring predialysis creatinine and documenting urine output. The phrase good urine is often used in practice. Early on, the urine output may be robust, but clearance is suboptimal.
The practice points related to withholding erythropoiesis-stimulating agents (ESAs), iron, and phosphate binders are also important to consider, although the level of evidence to support recommendations is quite limited. In my own practice, I have often started the patient on regular ESA therapy during dialysis (after repleting their iron) while they are an inpatient. Anemia may increase the risk of IDH. Besides, allowing the patient’s hemoglobin to drift down increases the risk of the patient requiring a blood transfusion, thereby sensitizing a patient who may otherwise be a good candidate for transplant. With regard to metabolic bone disease treatments, the value of withholding phosphate binders or vitamin D3 seems largely opinion based, and I have tended to manage this among inpatients by starting both a phosphate binder and vitamin D3 if they are needed.
In summary, the term dialytrauma used in the new recovery from AKI-D context is a useful addition to the dialysis team’s lexicon. It fundamentally relies on the Oslerian idea of “record, tabulate, communicate.”
References
1. Barreto EF, et al. Kidney360. 2024;5(1):124-132. doi:10.34067/KID.0000000000000309
2. Vijayan A, et al. J Am Soc Nephrol. 2025;36(5):926-939. doi:10.1681/ASN.0000000646
3. Davenport A. Kidney Int Rep. 2022;8(3):405-418. doi:10.1016/j.ekir.2022.10.031
Note: The opinions expressed in this column are the contributor’s own and do not represent those of Nephrology Times.







 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.