Dr. Jeremie Calais on FAP-Targeted PET Imaging and Molecular Radiotherapy in Cancer Patients
By Rob Dillard - Last Updated: April 27, 2023Jeremie Calais MD MSc, Associate Professor, Department of Molecular and Medical Pharmacology, Director, UCLA Theranostics Program, Ahmanson Translational Theranostics Division, University of California, Los Angeles, was great enough to share his vast knowledge on FAP-targeted PET imaging and molecular radiotherapy in cancer patients. His presentation was both informative and attention-grabbing. See what Dr. Calais had to say.
Dr. Jeremie Calais: Hello everyone. Thank you for joining this presentation. It is my great pleasure for me to share my experience with the FAP-targeted PET imaging and molecular radiotherapy in cancer patients. So just to be sure, we all on the same page before we start talking about FAP and FAPI today, we’re going to talk about the stroma. The stroma can be seen as kind of a, the reaction of the host to the invasion of the cancer cells. The cancer cells induce a wound healing response. This response associated with some inflammatory changes can be called the tumor stroma, the desmoplastic reaction, the tumor micro-environment, or cancer fibrosis.
And of course, this has great properties for targeted treatment or imaging and it’s a target of high interest for the whole oncology community. One of the main cells content in this trauma is the cancer-associated fibroblast, the C-A-F, CAF. And this CAF, they express a lot of protein called FAP fibroblast activation protein. And now we have radiopharmaceuticals that are specifically designed to bind into it with high specificity to either deliver beta positron radiation, to be used for PET/CT imaging, or even now people are thinking of using it for treatment by delivering alpha local radiation or beta minus radiation. That would be the ultimate goal of FAP-targeted radiopharmaceutical therapy.
So when you look at the gene expression of FAP in the protein atlas, you can see that the level of expression is very low in almost all organs, except the uterus; for some reason, at some background level all the time. And transform fibroblasts or the activated fibroblasts, they have a very high-level expression. So just by looking at these graphs, you can guess that if you have a way to get there, you will have either a very contrasted imaging agent or a drug with a very high therapeutic index with low uptake or low type distribution into normal organs.
And so that target is in fact known for quite some time. For example, in the 90s, there was already some attempts to use this target for radiopharmaceutical delivery. And here is an example of radio immunotherapy with iodine131 with using antibody F19. That was a specific for FAP. You can see these images kind of vintage of spec CT of FAP expressing liver metastasis, and the planar images obtained with iodine131. But a little bit like with PSMA or DOTATATE this was not really for prime time. There was not really PET/CT it was antibodies only. So what make really the difference during the past years of [inaudible] the creation of all these small peptides, low weight molecules that have maybe much better properties for targeted imaging, because they’re smaller, they go very quickly from the blood to the targets.
And so they’re much easier to use than big antibodies. And our colleagues in Heidelberg, they have a great radio chemistry research development team over there, and they developed this quinolone-based class of radiopharmaceutical called FAPI. So the “I” stands for inhibitors and you probably all have seen these very impressive images with great contrast, high tumor to background ratio, black on white lesions to background. This came out maybe in 2018, 2019, there was a lot of hype. At the meeting of the annual meeting of the SMI in 2019, since then there were multiple publications, multiple, let’s say editorial interest saying will FAP replace FDG or not. And so it generate lot of hype. When you look at PubMeds, I did a search on in February 2022. So now I think we’re in March.
So it may have increased again, significantly. You can see that it started in 2018, and now we are reaching close to 300 papers. I have to say most of the papers there are in fact case reports. There is not a lot of good, big prospective trials with big cohorts. It’s either retrospective studies or case reports. It’s interesting to see where these are coming from. Mostly China you can see more than half of them. Then from Germany, the creators kind of. Turkey they did a lot, they did quite some. And then the USA, India, Thailand, and Iran, these are the countries where there has been some experience with FAPI PET/CT. In the US now, if you want to do something with FAPI PETs, you have to go through a company. They acquire the license of the FAPI compound in 2019. This is SOFIE from Heidelberg university, and now they just recently have obtained an IND to perform clinical research using the FAPI PET/CT compounds. There IND will be initially valid for pancreas cancer study phase two trial.
At UCLA we started way before that, and we had an agreement between Heidelberg and UCLA. We used a different regulatory pathway than the IND to conduct clinical trials. We used what we call the RDRC. It is another regulatory pathway that allows the use of a new tracer, a new radiopharmaceutical in human, with or without all the preclinical required data that is usually asked for in IND. So it allows the use of that in patients in human, but you cap in terms of the number of patients you can do. And also in terms of diagnostic efficacy parameters, you can prospectively assess. So these studies are mostly exploratory studies, biodistribution studies, in which for you just administer a new tracer. And you basically look at the biodistribution. You can see here that we have various cancer types allowed in these studies. We have now enrolled 65 patients as of early 2022. The aim of this study, because we’re not allowed to talk about pure diagnostic efficacy with predictive value, sensitivity, specificity.
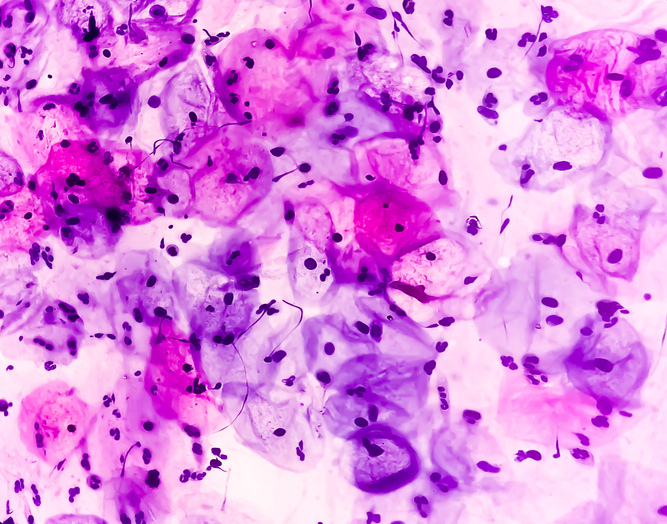
Here we aim at validating the biodistribution of the tracer with the immunohistochemistry of the FAP expression of the target expression by immunohistochemistry. So we recruited patients who are scheduled to undergo surgical recession of their tumor. So only patients scheduled to undergo surgery. The recruitment is hard because you need to squeeze in a scan in a patient who already had a PET/CT scan FDG before, who is scheduled for surgery, and you need to squeeze in a FAPI PET scan that would basically have no impact on his clinical care. So the recruitment’s a bit slow, but we’re getting there and we can generate nice correlation between IHC scoring and SUV from this dataset. We have recruited 65 patients, as I said before, you can see here the various cancer types that we have so far. We have strong collaboration network with our prostate cancer and sarcoma colleagues specialists.
So that’s why there is this, these high numbers in these cancer types. We have published recently a primary analysis with the first 15-patient analysis. These patients were recruiting between December 2019 and May 2020. You can see here, the various cancer types, mostly colorectal cancers. They all had surgery within, let’s say almost kind of close to two weeks after the FAPI PET scan. Underwent surgery and that we did we look at the uptake of the primary tumor. You can see here, an example of a sigmoid colon adenocarcinoma with very intense FAPI uptake. We look at the staining, you can see the FAP IHC staining of the cancer tissue here; and we look at the adjacent to the tumor region, and we compare the SUV in this adjacent region within the normal region on the same slides that was obtained in pathology. Here is another example where you see the primary tumor, very focal, intense uptake in this colon adenocarcinoma. And then we take the SUV in this normal region close to the tumor. And we look at the IHC current in the region adjacent to the very strong IHC scoring system in this FAP expressing region of the primary tumor. And the highest FAP immunohistochemistry score were observing pancreatic, esophagus, and breast cancers. The FAP stain was exclusively confined to the tumor associated stromal compartment in most of the patients.
And what was very interesting is to see that the staining intensity was greatest in stromal areas that were either within or immediately adjacent of the malignant compartment of the tumor. So the closer you are to the tumor cell, the FAP expression there is, and the further you are, the less FAP expression you have. And in the non-cancer tissues, when you do see some FAP protein expression, it was primarily observing capillary and small vessel endothelium. So this may be important to know for the future. When you look at the correlation, you can see that what you see on the scan, the signal intensity as assessed by the SUV and the IHC scoring system that was graded by two independent pathologists correlate nicely. So the more you have FAP protein expression, as it says by IHC score, the more intense is the signal on PET. And when you look at the cancer lesion versus the non-cancer adjacent tissue, that I just show before you can see that the signal both on the IHC scoring and the SUV is higher in the cancer than in the non-cancer adjacent tissue, very close by.
And now we’re getting close to 70 patients done at UCLA. So we are learning how to read these scans and biodistribution of FAPI PET tracers. And there are some interesting things to be known before we can move further. I like this example here, this is a five year cancer patient. You can see the primary tumor in the distal portion here, and this patient underwent resection and got his whole as a removed and analyzed for pathology. All these parts, the meat portion here was in fact not cancer and just fibrotic or inflammatory changes. Of course, when you look at that, it’s pretty hard to make a difference and make a final call on the read.
So we start to see many non-oncologic findings that we reported. You can see here, the breast’s tissue can have strong FAP expression under certain hormonal conditions. I will go back on that later. You can see that any granulomatosis process, any disease like tuberculosis, sarcoidosis that induce granulomatosis or inflammatory process can induce a strong FAP activation and expression. You can see that thyroiditis this as well can have a strong signal on FAPI PET. There are now two papers that I like very much to describe all the non-oncologic findings that we could call pitfalls in the context of cancer application, but we can only also use it for non-oncologic applications. Of course, today I’m going to talk about cancer patients. So I will call it pitfall. You can see that inflammatory lymph nodes like with these pitfalls I think they are many of them they are unspecific to a tracer.
You see that with most of any nuclear medicine tracer at the end. So inflammatory lymph node, osteoarthritis, hemorrhoids, fractures in the bone, the vision narrative changes, the inflammatory changes, esophagitis, pneumonia, all that you see, and they are nicely summarized in that paper. It is actually what we use as well in our cohorts. So if you put the same graph that I just show you before, when we look at the IHC staining and the FAPI SUV on a selected sample, you do the same, but this time you compare all these benign uptake and you see that you have a significant overlap of FAPI SUV for cancer lesions or benign lesions or inflammatory lymph nodes versus malignant lymph node. So of course, FAPI and FAP is not specific to cancer. It is just fibroblast activated.
In this nice paper it is a more pictorial there’s images. So I choose to display that here it is done by our colleagues in Essen, that summarized pretty nicely what was in the table before and are experience as well in our patient of 70 patients at UCLA. So in the salivary gland, there is a little bit of level of expression at various level. I think it depends on the prior history of the patient in terms of salivary gland exposure to potential traumatic causes. Interestingly, the optic and ocular muscles have some signal, so that’s interesting to observe as expected anything in the mouth that is related to dental implant, dental extraction, any gesture in the mouth would induce some kind of expression of FAP and reactional processes, all the scar tissue, the remodeling in the muscles. You can see here, that’s probably a contractor or, some muscle benign inflammatory process that induce fibrotic reaction. This is the most common one, I think, classical the degenerative joints and bone findings that you can see here. You see on the left temporomandibular joint here in the spine, in the posterior processes here, also in the spine anterior processes. And here, interestingly, you see a very focal and strong signal in intraspongious hernia, you see that FDG there was nothing, and there is some FAP expression in rest equipment in that.
Yeah, I like to show this example because this lesion, which was of course, very suspicious of cancer, depending on the indication the SVMAX was 14, as you can see here was biopsied then was in fact, a tuberculosis granulomatosis inflammation patient responded well to anti infectious treatment. But just to show you that anything that creates some fibrosis and remodeling of the microenvironment surrounding a lesion would enhance the FAP expression and have a strong FAPI signal on PET. The hormonal status in specifically female patient but probably also in male may influence the uptake of some organs, such as the breast or the uterus and the endometrium here. That’s very normal to see the uterus like that, and also the breast. And they really, depending on the hormonal studies of this can be sometime very intense. You can see here, the SUV in premenopausal patients versus postmenopausal patients. One of the main pitfalls, and that specifically when a patient will be interested to look at pancreas cancer indication is the pancreatitis. The pancreatitis, the inflammation, and the fibrotic processes that occur in the pancreas and you have a lot of FAP overexpression mechanisms.
And you can see here, tissue uptake in patients with pancreas disease. That’s pretty frequent to see that specifically in a patient population with suspicion of pancreas cancer. So people have tried to get rid of this background signal. Diffuse by doing late imaging acquisition, you can see here, two studies showing images over three hours and you have more or less a stable uptake in the tumor lesions; whereas the background pancreatitis parenchymal uptake decreases over time. So it’s over always a little bit like with FDG or with any other tracer often in cancer imaging, you do late imaging and you try to get this differential uptake time.
What is interesting in that study is that they look at 100 patients with even focal uptake in the pancreas. They found seven cases. They follow all these cases. And at the end, all the pancreatic lesions were proven to be non-neoplastic. So the cysts pancreatitis IGG four, but even when it’s focal, it doesn’t mean it is cancer when it is in the pancreas. So that’s a clear pitfall here to be known. So the questions that come all the time now that I’m usually asked is, what is the killer indication for cancer imaging and diagnostic? We start to have to see some meta-analysis and review a little bit in permit from this amount of literature that is available. But of course, like I said, there is mostly retrospective studies case reports. So the data quality is not excellent.
And when you have on the patient-based analysis, sensitivity of 99%, primary tumor 100%, I mean, these numbers show just a strong patient selection bias. And that maybe the question asked to the diagnostic purposes while maybe not appropriate in a real life manner. I think these numbers would be very different once we start to do true prospective trials. Let’s look at it a little bit when you compare of course, FAPI versus FDG, because everybody’s talking about how can FAPI replace FDG. It started in 2019, I put here all the studies that have intra-patient comparison of FAPI and FDG. So patients who underwent both scans more or less at the same time, that have reported fighting and not independent cohorts. So in that study, there was six patients in Germany. Then lot of Chinese studies, 75, 68, 123 Turkish studies here, another German study, a multicenter study that pulled data from Germany, UCLA, and South Africa and a review.
And when you try to extrapolate that and extract a little bit of a signal from all these studies, it’s not easy at the end, they report mostly the differential SUV between organs, between lesions, head-to-head. And so clearly you have a higher tumor to background ratio of FAPI over FDG in many situations, specifically in organs, where you have high FDG uptake as a background normal, such as in the brain, the oral mucosa, the liver, the gastrointestinal, or digestive, there is always like some background activity. And sometimes the just FDG signal of the tumor lesions can be low or in the bone, which is a common limitation of FDG PET imaging. So these are observed and these are pretty clear. So that’s a given what is unclear is how these properties can translate into actual, useful improved diagnostic performances.
And it seems from the studies that are published and all the case that are reported, that there may be a potential superiority of FAPI for metastatic detection in bone, brain, liver, and the peritoneal carcinomatosis, and for the primary detection of this cancer type breast, cholangiocarcinoma, gastric cancer, head and neck cancer, or pancreas cancer. I will display a couple of examples here that I personally choose. So it’s completely biased towards my opinion, and basically tell what I think that may work. So let’s look first at the bone metastatsis detection in that study, they reported the FAPI and FDG SUV in osteolytic and osteoblastic lesion of almost 100 patients for each. And you can see that in these 100 lesions, the SUVmax was higher with FAPI than with FDG. However, there were more FAPI false positive than with FDG.
And this echoes to what I just show before with this strong reaction in some degenerative processes, for example, the granulomas’ pitfall that I show before. Here is just a nice example when you see a more micro environment reaction and FAP expression in these lesions than with FDG where just purely see the obliquethetic activity of the tumor, which is often lower in bone metastasis. So potentially better for bone metastasis detection, liver metastasis can be very tricky with FDG. And even with MRI sometime. In this little study, 31-patient retrospective that were kind of basket staging, restaging indications, they all had metastasis in the liver from colorectal cancer, pancreas, or gastric cancer. You can see the different tumor types that were included in that study. Well, you can see that the SUV with FAPI is a little bit higher than with FDG, not that much, but a little bit. But you can see more importantly that the tumor to background ratio are much higher with FAPI than with FDG.
And so that’s maybe the difference in the liver. And there were 29 cases positive with FAPI versus 22 with FDG. So there were eight cases that were negative at FDG and positive by FAPI. So potentially a good role, especially in gastric cancer. Maybe it seems that is where there is the highest signal for liver metastasis staging. Peritoneal carcinomatosis this can be tricky sometime this can upgrade patients to a very important staging information for treatment direction and surgical management. And in a study that look at 46 patients, which suspected peritoneal malignancy, there were a median SUVmax of 3.5 with FDG versus nine for FAPI. So it seems that the peritoneal carcinomatosis induced much more fibrotic process and activation of fibroblast in particular in the gastric cancer subtype. The PCI score, which is a way of scoring the extent of the peritoneal carcinomatosis was much higher with FAPI than with FDG. And the sensitivity was also much higher, 97% and 72%.
So potentially a good role for peritoneal carcinomatosis detection as well. Now let’s look at some primary tumor, different subtype and potential indications. So pancreas cancer, as I said, the main study that will occur prospectively in the US. The first one will be in pancreas cancer. I saw that before. What has been published so far in PubMed is mostly again, retrospective study. Let’s look at them, here you have a 36-patient, which suspected or diagnosed pancreas cancer. Often in these retrospective studies, you have a mix and a basket of different indication, which is makes very hard to extract a strong signal from it. And you can see that FAPI PET scan upstaged six patients. So 26% of the cohort and change the management in 8% versus FDG. And when you compare it versus contrast enhance CT it upstage 20% of the patients and change the management in only one patient.
And interestingly, you can see that the intense FAPI uptake was observed throughout the procrea is almost half of the patient. So that may render difficulty actual usefulness in that setting, you can look at that. This was not mentioned, but 30% of specificity for FAPI that makes it quite concerning. So to get 100% of sensitivity, they have basically to call everything and the specificity decreases a lot. So maybe if we keep a good level of specificity, the sensitivity would be much lower. Another study here, 33 patients. So more or less the same size, the detection rate for primary tumor was 100% with both tracers there, again in half of the patient parenchymal uptake in the background observed only in 13% of the patient with FDG, there were more lymph nodes detected with FAPI, but there were more liver metastasis detected in FDG in that cohort.
So at the end, it is a bit unclear how it would be easy to prove or not, that FAPI can be really useful in that setting. And they conclude with that MRI’s required for primary tumor and liver staging in any case, and MRI would be hard to beat. In that little series of 19 patients, they look at the impact on management, just on FAPI versus contrast enhance CT. The TNM stage was changed in half of the patients. These patients had either newly diagnosed or recurrent disease. And this change of TNM lead to management change in 36% of the patients. So you still see things on the scan that are maybe helpful for your management choice. But to me, it will be very difficult to show all these data prospectively. Let’s look at an indication that for me, will probably work pretty well.
It is the gastric cancer. Let’s look at this first series, 10 patients, the detection rate of the primary tumor that is usually let’s say low with FDG. Here it was 100% with FAPI, 50% with the FDG, the SUVmax was much higher; you can see 16 versus five, and more importantly, the TBA was also much higher because often with FDG, you have this gastric wall signal that makes the read very difficult, almost impossible. And so the detection of original lymph node was comparable and the peritoneal carcinomatosis was detected more with FAPI than with FDG as I suspected. Another series here of 20 patients, you can see that FAPI PET was superior to FDG for primary tumor, and again, peritoneal metastasis detection. And you can see that FAPI and FDG were equivalent for lymph nodes, liver, bone and ovarian lesions. Here in red are all the FAPI intensity signal or is to read for different regions.
And here in blue are ones for FDG. So you can see that for most of the cases and regions, FAPI show the most intense visual scoring system. In this bicentric retrospective analysis that included 38 patients, for the detection of primary gastric cancer, FAPI sensitivity was 100% versus 80% for FDG; and metastatic lesions, 60% for FAPI versus 50% for FDG. So it seems that this higher tumor to background ratio as shown here can enhance maybe the detection of primary tumor and also metastatic lesion in this gastric cancer staging so that may be a good one.
One other that I like personally and is the cancer of unknown primary, because I think there is a strong unmet need, and there are some early reports. For example, in this 18-patient cohort with all FDG negative scan, you can see here, the bilateral uptake that makes… Yeah, you don’t know if there is asymmetry or not. Where on the FAPI scan, it was clearly on the right side. So the primary tumor was detected here. And at the end, they detected almost 40% of the primary tumor in patients who had prior FDG negative. You can see though that the level of uptake is in the same range, but the TDR may be a bit improved. So that’s promising data, but in this other series of eight patients, the primary was identified by both FAPI and FDG in all eight cases. So again, if you have to do that prospectively, it may be promising, but it may be hard to really demonstrate superiority prospectively.
Breast cancer – there are some early reports that show nice uptake, nice expression of the target FAP in the primary tumor across various disease stage and subtypes. Same in the lymph node metastasis, you can see here this black and white lesion, both in the primary tumor and the lymph nodes in this cohort of 18 and treated primary breast cancer. So there’s maybe a good potential here, but again, you will have to beat FDG and beat other modalities such as MRI, that may be not easy in this little retrospective study of 50 patients, almost so good numbers. The uptake seems higher. You can see that the FAPI uptake is much higher than the FDG uptake, but at the end, because it was a basket study without any clear diagnostic accuracy endpoints, the staging on impact was really unclear. They just show that the uptake may be higher and that may lead to change in stage. More or less the same findings here in 20 patients, where the sensitivity was higher with FAPI, you can see that the specificity was a bit lower in the breast.
You have some changes so that can be a pitfall. They report higher FAPI TBR, higher FAPI SUV. But again, the staging impact was unclear. And I think the last one I’m going to talk here is the sarcoma indication in this paper with the 45 patients with recurrence of tissue sarcoma. You know sarcoma is a very heterogeneous box of disease where you have many subtypes that behave very differently depending on their grade. And I highlighted it here in red, the ones in which FAPI is very strongly expressed by both probably also the cancer cells themselves, because it’s a fibroblast cancer potentially. And in blue, the ones with much more FDG uptake. And it seems that for liposarcoma, malignant solitary fibrous tumor, interdigitating dendritic cell sarcoma, FAPI can be much better than FDG. And on the other hand, undifferentiated polymorphic sarcoma or rhabdomyosarcoma, there seem to be much better with FDG. The low-grade tumor G one also much more intensely seen with FAPI than with FDG.
This I can clearly confirm in our cohort as well in UCLA. In this study done in Germany, they try to assess the impact on management of patients who undergo FAPI PET imaging for bone or soft tissue sarcoma. Again, it was a basket trial with staging or restaging indication. They correlate nicely that the FAPI SUV and the FAPI IHC score correlates. When you have high FAPI IHC score, you have high FAPI SUV and the reports a change in management in 30% of the patients. These are 30% of the patients with the management change. Now, when you look at the detection efficacy, the numbers look pretty similar between FDG and FAPI. So again, it is unclear to me how you can place FAPI in the diagnostic and treatment algorithm and show a prospectively, a good benefit. I think many studies need to be done and I look forward to see the results. One key thing and one, I think the main application for FAPI PETs is to act as a biomarker for FAP expression. In case, you have a good FAP-targeted therapy and if we talk about FAP-targeted radiopharmaceutical therapy, this FAPI PET will be, of course, the entry gate for any patient who is considering such therapy. We start to have like some kind of reports in PubMed on the early experience of FAP-targeted molecular radiotherapy. In February, I was able to kind of extract the data from 65 patients in PubMed. So the experience started in Germany, of course, with about a dozen patients treated with etruim FAPI46 FAPI04. And then there were some patients treated in Iran, in China with lutetuim-177, about 30 patients with FAPI46 and FAPI04. Then there is the FAPI2286 compound that was developed by Professor Baum in Bad Berka. And I just recently reported in the… I will talk about that. And there is this new compound DOTAGA.SA.FAPI2 that is used in India. Now that I will talk about it as well.
So one thing that I try to look for is this kind of images PSMA molecular radiotherapy had very quickly an early hype. It was a blast right away. There was this case report showing this impressive response, both on serum markers and on images with this treatment coming from Germany. This started probably in 2015, same with actinium these very impressive images with great response, both by PSA and images. Well, I didn’t find anything like that with FAP-targeted therapy I tried to look for it. Here you have scans these are FAP scans before and after one cycle, two cycles, it depends. And you see, you don’t get these types of images. Here are even FDG. You can see the heart signal here, the brain signal, and you can see that the response by FDG is not great as well. So I wasn’t able to find these images just because they don’t exist.
And of course, if they would exist, they would have been published already a long time ago. Let’s look a little bit at the efficacy data that is reported in this early cohort. They usually have treated patients very end stage, very advanced. So it is difficult to get any types of response, of course, because these patients are very close to the end. So you can see here the type of response. There is no PR, no CR, you have some SD and some PD, similarly as well here, PD or SD, but no PR. Again, of course, it’s very advanced patients, so it’s kind of hard to get any types of response with any therapy, but we don’t see a good signal of efficacy. These studies were really made for visibility purposes and safety.
One of the main drawbacks I think that makes it for now not a successful approach is the retention time of the FAPI class compounds. They have a fast… Maybe they recirculate after they get internalized into the cell after binding. And so it seems they don’t stay a long time in the tumor lesion. And if you deliver radiopharmaceutical, that has a high flight, for example, like lutetium of about a week or about 10 days, or maybe you need more time than just a couple of hours to deliver the whole energy that you need to induce sufficient damage to the DNA. And when you look at images here, for example, you see this good target expression on the baseline PET, a good delivery of the retest FAPI-46 at 24 hours, but rapidly it seems to decrease over time after 72 hours, and it goes into the kidney and the urine. Same kind of images here in a pancreas cancer patient. You see uptake at the beginning, but then rapidly, you don’t see this very contrasted late images that you see like that with PSMA, you know that your treatment went there right away in a 24, 48, 72, nine days, you see the retention of the retest PSMA radiopharmaceutical therapy in your target continuously delivering radiation and reducing damage, and that’s why it works. And that’s probably maybe one of the reasons why it doesn’t work for now with FAPI with this fast recirculation time. So there is a high interest of the scientific community to improve the retention time of the FAP-targeted radiopharmaceutical therapy agents. There have been multiple attempts that has been made already so far there. One is to add Albruim Binders and to prolong the blood circulation time, and with more circulation time in the blood, not excreted into the urine. You give more time and differential time between increased continuous uptake from the tumor, whereas it’s flushed out from the normal organ. So that’s the theoretical concept and the aim. And there is also a way what that is called multimerization to increase tumor mutation. The binding motive or the targeting motive is doubled on the carrier. So you have two attachment ports to the target basically to be more attached and that the radiopharmaceutical stays there with two attachment link. There is also FAP-2286 which is a cyclic polypeptide linked to DOTA chelator. So it is not a quinolone based molecule. This one is owned by Clovis now in the US. This was developed by Professor Baum in Bad Berka. And you can see here that it seems that the retention is much better with increasing over time.
And the early human experience has been reported recently in the JNM; you can see the FAP expression with the FAP-2286 gallium compound. And then the scans obtained after injection of the treatment with lutetium FAP-2286. And you can see a very good, let’s say retention over time after 10 days; you see still good target retention. There is more kidney signal lately. So maybe we’ll have to see how this translates into a kidney toxicity or not. And if you look at the efficacy results that are published in this little cohort of 10 patients, again, there is no strong signal of tumor response or efficacy. It was again more about safety and visibility on the progressive disease. Because again, these patients were really end staged.
I like to show here that because I find that very interesting, this DOTAGA.(SA.FAPI)2 from the Indian studies here, you can see that after 168 hours, you still have a pretty good signal in the tumor lesions that you want to treat. And you see a very good response, both on the serum marker here. This was a case of radio iodine and refractory differentiated thyroid cancer. And you see a good imaging and serum marker response so that’s maybe the most promising image I was able to extract from PubMed. So this was in the thyroid cancer patient population. Here is another example with a really diffused lung metastasis of radio iodine refractory differentiate thyroid cancer. And you can see that this double-headed linker to the FAP target seems to work well because the radiopharmaceutical seems to stay there. And this was again with lutetium, and you can see that after 96 hours, you still have a good radiopharmaceutical retention in the targets.
And again, interestingly, you start to see some response based on various criteria, but there are some patients that seem to respond to this treatment with this FAPI compound so that’s maybe a promising approach. I think that was an interesting report from India. Of course, small cohorts, always very difficult to reprove prospectively. And if you look at the dosimetry and trying to understand a little bit more per lesion and what these compounds can deliver as energy for radiation. You can see that for the kidney is pretty safe. I put here the lutetium PSMA, the lutetium DOTATATE, the commonly approved and use one just for comparison. So you see that there is kind of more activity in the kidney, so the FAPI compound maybe more worrisome in terms of kidney toxicity, and this can have an impact for the FDA and all the regulatory approval of course. The bone marrow toxicity is very low, there is no bone marrow uptake a lot. And when you look at the tumor doses, of course, there is always a pretty significant range in the different values that are given in all these studies. Usually the classical one that are retained is like something between three to five Gy/GBq for lutetium PSMA lutetium DOTATATE. This is usually in the range of one with Y-FAPI-46, Lu177-FAPI-46. It seems that it’s three. It seems to be better with FAPI-2286 lutetium. And interestingly in the DOTAGA.(SA.FAPI)2 it was 10 so much higher in that reports. So maybe that’s promising.
And it was kind of interesting for me to observe all this rush of all the companies to get license all this new FAP-targeted radiopharmaceutical compounds. There are multiple players in the market now. They all have virus compounds. So it would be very interesting and exciting to see all these attempts and the future in the next three, five, four years with all these new compounds. With that and thank you very much for your attention. I hoped you enjoy the talk and feel free to send me an email if you want to ask me any question about FAP-targeted theranostics. Thank you very much.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.