Dr. Holstein: Targets of Interest for the Treatment of Multiple Myeloma
By Kerri Fitzgerald - Last Updated: April 10, 2023Sarah Holstein, MD, PhD, associate professor of medicine in the Division of Oncology & Hematology at the University of Nebraska Medical Center, talks about BCMA as a target of interest for multiple myeloma (MM), as well as other emerging targets.
In part three of this interview with Dr. Holstein, available November 17, she discusses disparities in clinical trial patient populations and how COVID-19 has impacted patient care.
Watch part 1 of the interview with Dr. Holstein where she discusses the MM treatment pipeline.
DocWire News: BCMA has emerged as a target of interest in multiple myeloma. First anti-BCMA agent, belantamab mafodotin, was recently approved for relapsed disease. And the FDA recently granted priority review for ide-cel, a BCMA-targeted CAR T-cell therapy. So can you talk about BCMA as a target and your thoughts on some of these agents?
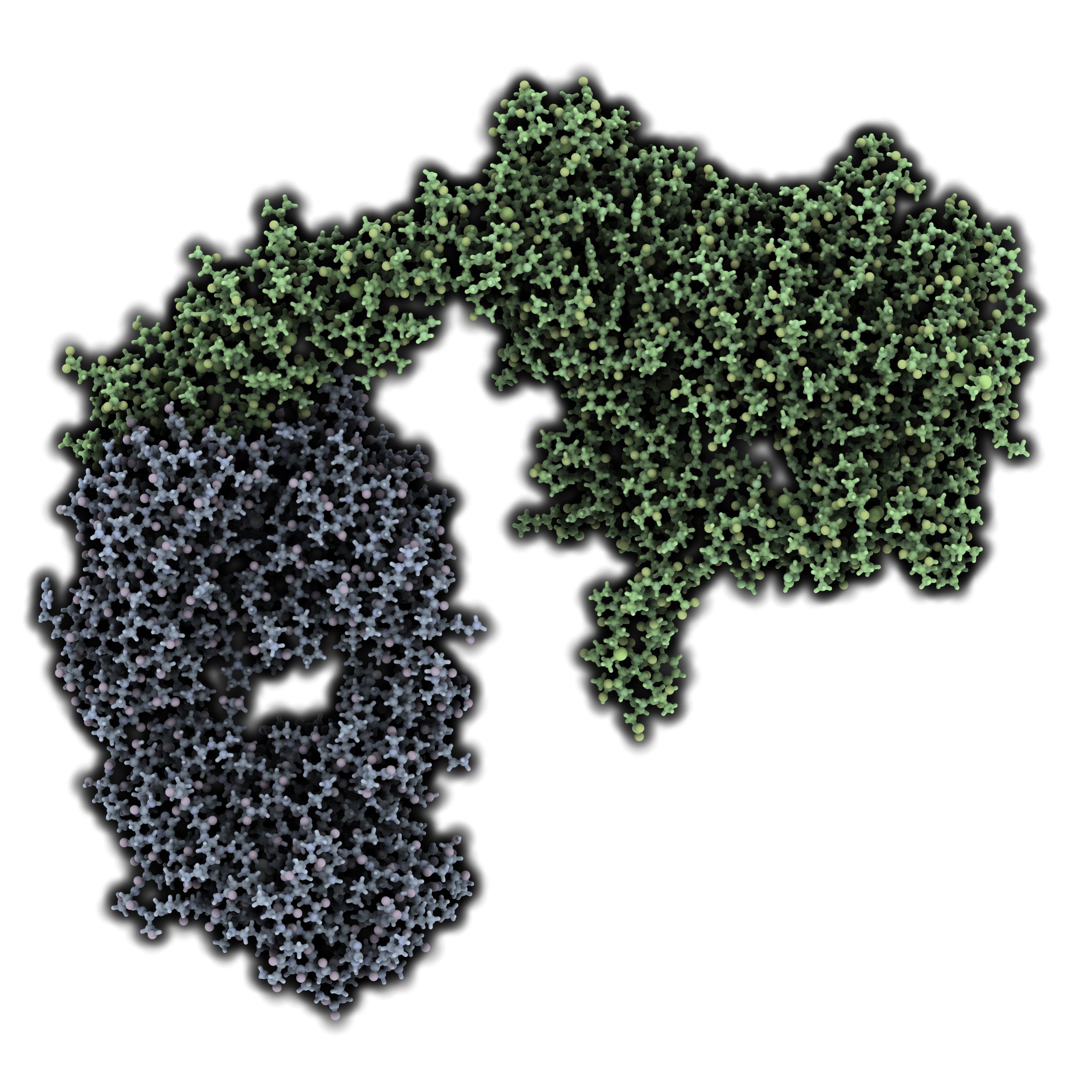
Dr. Holstein: It’s great that all the preclinical research identified BCMA as a target, because we really needed new targets in myeloma. BCMA is very attractive because it is so highly expressed and almost uniformly expressed on most malignant plasma cells. It’s not 100%, but the vast majority of myeloma cells do express BCMA. And there’s not a lot of off-target expression in terms of things aside from B-cells. So that makes it a very attractive candidate for targeting for myeloma specifically.
It’s proven to be an attractive candidate as well, because we now have multiple different ways to target it, both from an off-the-shelf antibody-based approach, as well as, of course, chimeric antigen receptor T-cells.
I think what’s been disappointing in the BCMA arena so far is the inability to simply develop a naked antibody, for example, like what we have with daratumumab. So that was, at least from the initial studies, proven not to be effective enough, and so other modalities have had to be used in order to get enough efficacy either by conjugating it to a toxin, as is the case with the ADC belantamab, or by using approaches through either bispecific T-cell engagers or bispecific antibodies and dually targeting CD3 T-cells at the same time.
The thing about BCMA that makes it a little bit more complicated is that it does get cleaved and shed from the cell surface. And so it’s clear that we need to start to work around some of the resistance mechanisms that are happening to all of these BCMA-directed therapies. I think one of the exciting and interesting approaches that was presented at last year’s ASH Meeting was a small study looking at BCMA-directed CAR T-cells in combination with a gamma secretase inhibitor. Gamma secretase is an enzyme that can cleave BCMA from the cell surface, and that soluble BCMA can act like a sink to sop up the therapeutic drug that we are delivering, which then limits the amount of drug which gets to the plasma cell where it needs to be.
So developing approaches that really work around the BCMA resistance patterns, I think, will be critical as we move forward to be able to maximally benefit from the variety of BCMA-directed therapies that are under development.
DocWire News: Are there any other targets of interest that clinical trials are looking at for multiple myeloma?
Dr. Holstein: There are a number. One new class of drugs, or at least relatively new class of drugs, are the CELMoDs, which are related to the IMiDs, the immunomodulatory drugs. So the CELMoDs still target cereblon, but there’s some chemistry involved and differences in specificity with respect to how they’re interacting with the E3 ubiquitin ligase, which make them very interesting.
There’s two so far that we have some clinical data for. The first one actually has a name, iberdomide, and there’s a lot of interest in that drug because it does show some efficacy, even in patients who are pomalidomide-resistant, which is a huge need for our patients. And then there’s a second one that does not yet have a name, which likewise in phase I studies has shown efficacy so far, even in patients who were pomalidomide-refractory.
The interesting thing about these agents will be, presumably, how hopefully easily they will be able to be partnered with some of our other existing therapies, particularly monoclonal antibodies. We know from the IMiD perspective that there’s synergy between monoclonal antibodies and IMiDs, and certainly there’s preclinical data as well that would suggest that that applies to the CELMoDs. There’s also interest as to whether or not these CELMoDs could improve CAR T-cell efficacy as well. So that makes the CELMoDs particularly interesting from my perspective.
Melflufen, I think, is another interesting agent, which is being evaluated by the FDA this year. And although it seems like an old agent with respect to the fact that at heart it’s an alkylating agent, there’s certainly preclinical data as well as clinical data, which suggests that it’s significantly more potent than a standard alkylating agent, with a better safety profile with respect to be able to more selectively deliver this novel alkylating agent to plasma cells. Again, this might be an agent that could be partnered with some of our other therapies quite readily. And so therefore would be of interest beyond just this use, as a doublet in combination with dexamethasone.
And then with respect to other targets besides BCMA for CAR T-cell, first, there’s the approach of dually targeting. So we’ve seen abstracts already of targeting both CD19 and BCMA to go after the presumed stem cell, as well as the more mature plasma cell. There’s the approach of really going after the whole axis of other BCMA family members. So taking the approach of designing CAR T-cells that behave more like APRIL and can bind to both BCMA and TACI to more effectively target that signaling pathway.
There’s, I think, some interesting preclinical data for GPRC5D as a truly novel target. It’s a protein which is found to be expressed on myeloma cells and also in hair follicles, but so far it doesn’t seem to be expressed elsewhere. So I know that there’s CAR T-cells under development for that as well.
The exciting thing is that we probably are just in our infancy with respect to developing CAR T-cells. And then as well, we’re moving beyond T-cells. There’s interesting preclinical and clinical data suggesting that both NK cells either unmanipulated or manipulated to have CARs on their surface could be a nice alternative to a T-cell based therapy.


 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.