Dr. Dan Bloomfield, Anthos, on the Benefits of Abelacimab
By Rob Dillard - Last Updated: September 6, 2023DocWire News recently spoke with Dan Bloomfield, MD, FACC, FAHA, Chief Medical Officer of Anthos Therapeutics. Dr. Bloomfield spoke about abelacimab, a Factor XI inhibitor that stands to greatly benefit patients with blood clots.
DocWire News: Tell us about your background and your role at Anthos Therapeutics.
Dr. Dan Bloomfield: Sure. So I’m a cardiologist, spent the first part of my career on the faculty at Columbia doing research and seeing patients, then I joined Merck, where I worked in drug development for 15 years. I joined Anthos three years ago as Chief Medical Officer.
What is abelacimab and what programs are you developing it in?
We’re developing abelacimab right now in two indications. One is in patients who have cancer and develop blood clots. The second are patients that have an arrhythmia of the heart, the heart’s not beating properly, blood clots can form in the heart, break off and go to the brain, causing a stroke. Those are our first two programs that we’re developing abelacimab for.
Blood clots are one of the leading causes of death, even with available anticoagulants in the market. What do you think is the reason for that?
There’s a couple of reasons. One is that sometimes blood clot’s the first presentation of a disease. You don’t even know you have it, or you’re at risk for it. There’s no way that we can prevent that. We can prevent subsequent clots, but that’s one reason.
An important reason for us is that there are patients who are at risk for blood clots who are not taking anticoagulents. We know that anticoagulants would help them, but for a variety of reasons, they’re not taking them. Some of those reasons might be they just had a bleed and they’re in the hospital from bleeding from an ulcer, or a elderly frail person who might fall. Doctors and patients may feel like they don’t want to take the risks of having significant bleeding, so they accept the increased risk of having a stroke.
It turns out, in atrial fibrillation, somewhere between 30 and 40 percent of patients are not being treated with an anticoagulent. And one of the questions that we’re asking is, how do we protect those patients? How can we create an anticoagulant that would be helpful to them, that would stem the risk of bleeding and still let them have prevention of blood clotting and strokes.
What are the benefits of Factor XI mediated anticoagulation over current available options?
The benefits of Factor XI are interesting. They’re based on the observation that patients without Factor XI, born without Factor XI, are protected from the risk of stroke or blood clots, but they have a normal bleeding phenotype, they bleed like everyone else. Unlike for example hemophilia, where you lose Factor VIII and you bleed terribly.
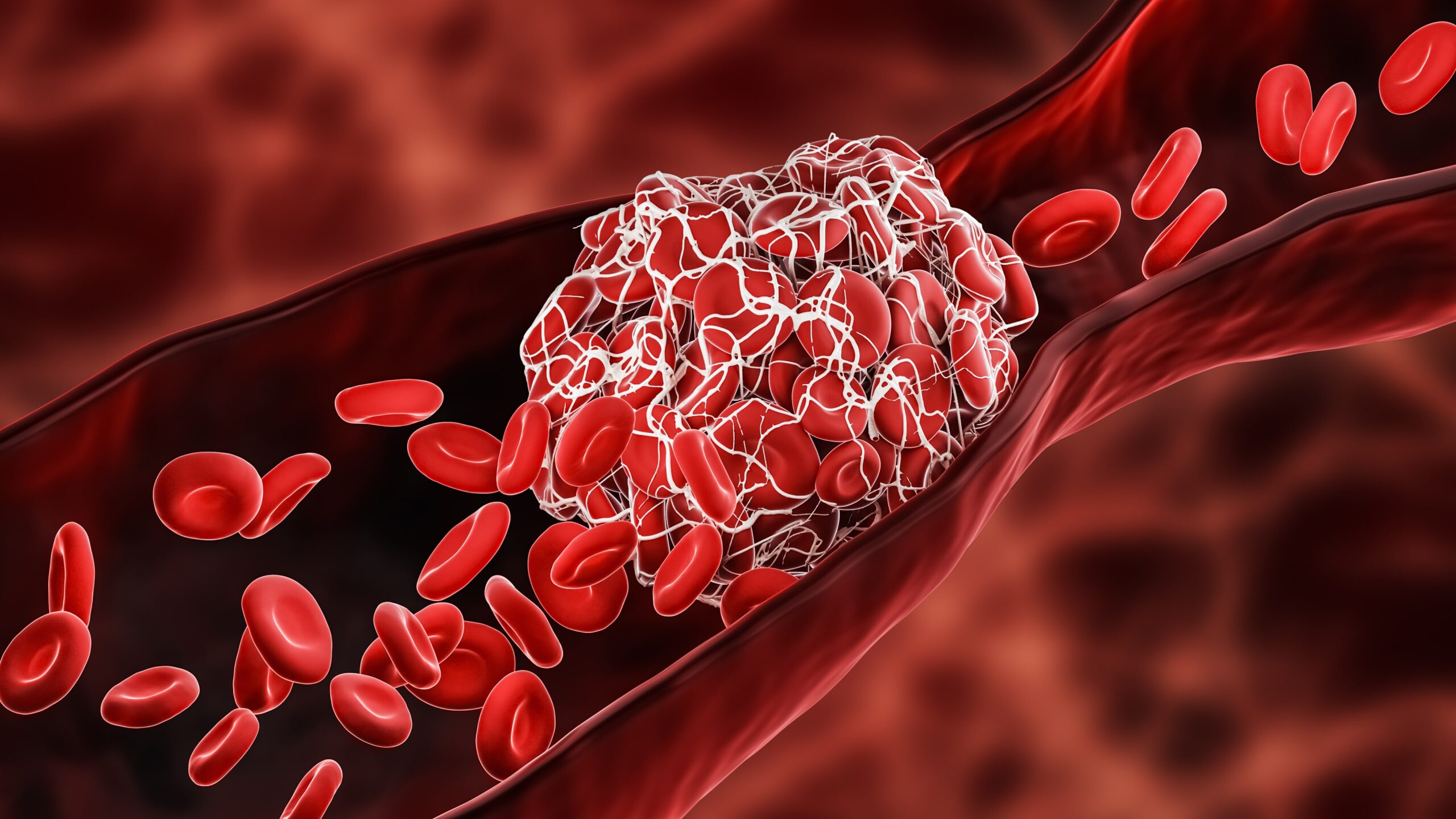
So it’s interesting that with patients with Factor XI, you don’t see a lot of bleeding. And that leads us to the conclusion, or the observation, that maybe you can inhibit Factor XI with a drug, prevent clots from forming, but not cause an increase in bleeding. We call that hemostasis sparing anticoagulents.
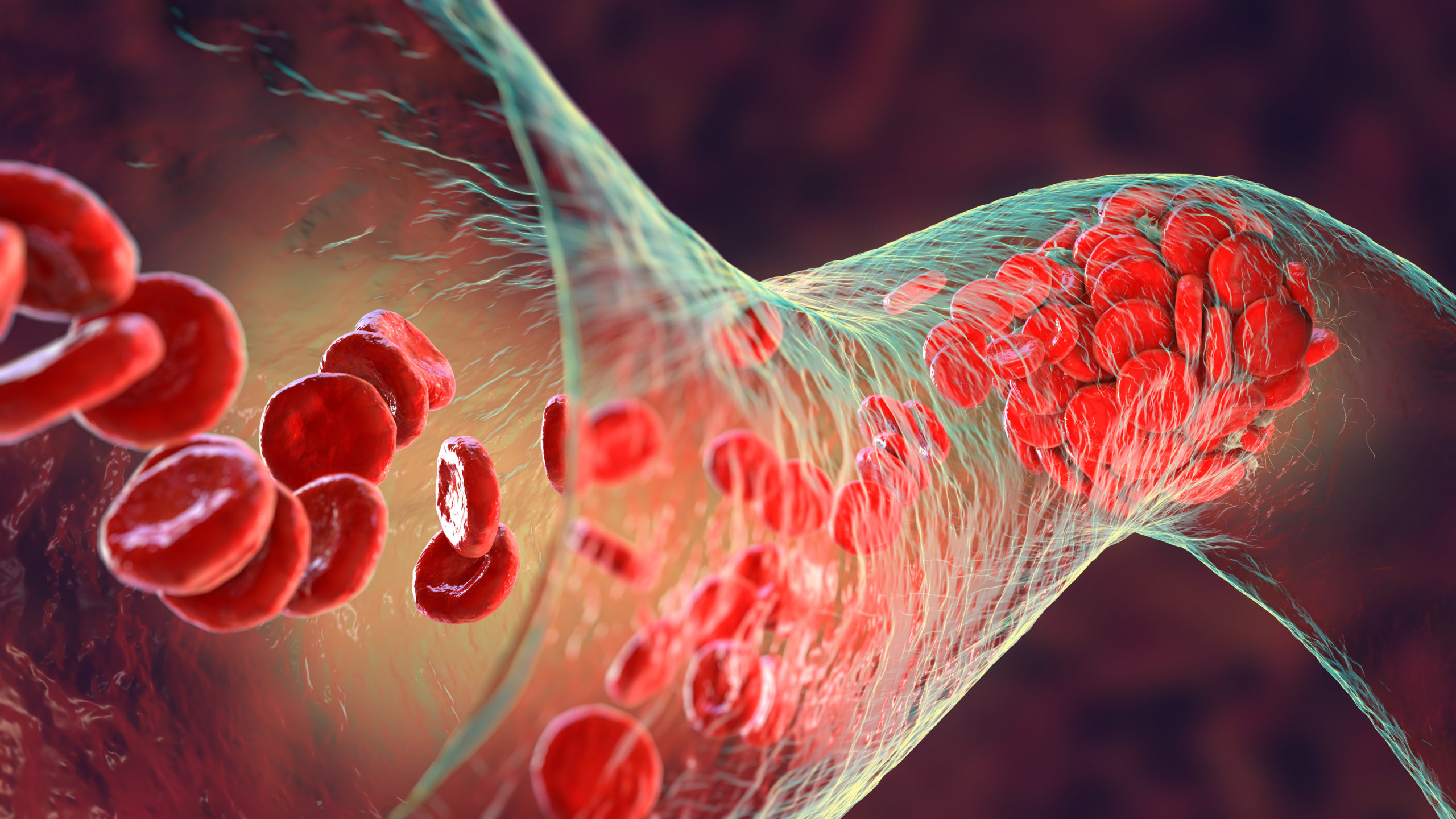
Hemostasis is the normal process where the body makes a blood clot to stop a bleed. If you can spare that process, so that process occurs normally, but anticoagulent prevent abnormal blood clots from forming, that’s kind of the holy grail of the field. How do you prevent blood clots without causing bleeding?
Arterial and venous blood clots lead to different conditions. Will abelacimab be studied in all these indications?
There are many indications, and we’re starting with two. The first are blood clots in the legs that may go off and break off to the lung. Those are on the venous side, the veins, and we’re looking at those blood clots in patients with cancer. Patients with cancer have an increased risk of developing blood clots, and they’re primarily blood clots on the venous side of circulation. So in the legs, or they break off to the lungs, which is potentially life threatening.
In contrast, there are blood clots on the arterial side, and stroke is one of them. The brain needs blood to bring its nutrients together, and if you block the blood supply to the brain, that tissue is going to die. That’s the stroke. So in that case, the illness is preventing blood from getting someplace. It can’t go to the brain or it can’t go to the heart, because you’re blocking the arterial side with a clot. That’s the difference between the arterial and venous side.
What are the current clinical trials that are being conducted by Anthos?
Yes, thank you. We are starting a large phase three programming, patients with cancer who present with blood clots. These two large phase three studies will be the largest program ever done in patients with cancer who have blood clots, and we’re focusing specifically in one study on patients who are at increased risk of bleeding.
These are patients, for example, with GI tumors, with tumors in their gut, where the risk of bleeding is high, and so you don’t want to give them an oral anticoagulant, so you’re stuck giving them daily injections. But we think our monthly injection of abelacimab will be just as effective as the daily injections and cause less bleeding.
So we’re focusing on those patients who really are challenging because of the risk of bleeding. We’re also doing a study that compares abelacimab to one of a leading anticoagulents being used today, called Eliquis or apixaban.
So those are the two studies happening now in the cancer side of it, of the company. And we’re in the middle now of running a large phase two B study in 1200 patients with atrial fibrillation. That study is fully enrolled, we’ll have the result of that study that roughly a year, and the study’s comparing two doses of abelacimab to a commonly used anticoagulent called Xarelto.
The goal of that study is to show that abelacimab causes less bleeding than the current agents that are being used. And if that’s the case, that’s the promise of abelacimab. We’ll need to do larger phase three studies to show that abelacimab prevents blood clots from forming, but we’ll know going into it that there’s no increased risk of bleeding relative to the other agents.
That study, when it reads out, will lead to other phase three studies in atrial fibrillation that we’ll get started. So we’re a small and very busy company.
What is the connection between cancer and blood clots?
Patients with cancer are at increased risk of blood clots compared to patients without cancer. Patients without cancer can get blood clots, but the risk is higher. And that’s because there are certain processes that go on with tumor cells that can lead to an increased risk of causing the factors to come together that lead to blood clots.
There are a number of different ways that can happen, it’s not a single way. Some tumors cause more blood clots than others. But it is a situation where a patient who’s sick with cancer, they develop a blood clot, it’s devastating news, right? They’re in chemotherapy, they’re fighting for their lives, and now with good chemotherapeutic agents. But all of a sudden they get a blood clot in their leg or their lung, and now everything stops. Got to treat them with anticoagulent, get them protected. And it’s devastating for the patients. That’s the situation that we’re trying to prevent.
Any closing thoughts?
I guess I’m going to close by saying blood clots do kill a lot of people around the world, and there are treatments that are available to prevent those blood clots from happening. Our goal is to create a drug that is safer than existing drugs, so it causes less bleeding, but still is able to prevent blood clots from forming. That would address a huge unmet medical need, and could prevent a substantial number of patients from having clots.



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.