In low- and middle-income countries, visual inspection with acetic acid (VIA) is used as a low-cost alternative to cytology in cervical cancer screening. But for HIV-positive women, VIA provides suboptimal screening results; to mitigate this screening barrier, researchers aimed to establish the feasibility of screening with VIA plus digital cervicography with real-time consultation (VIA-DCRC) using smartphones to obtain high-quality images. This study, published in Gynecologic Oncology Reports, compares the screening performances of VIA alone versus VIA-DCRC for HIV-positive women.
The cross-sectional analysis included 200 HIV-positive women; in one arm, VIA was performed, and in the other arm, VIA-DCRC was performed. In the VIA-DCRC arm, a trained nurse did the VIA, captured an image of the cervix, uploaded it, and electronically shared it in real time with three blinded study consultants (gynecologic oncologists) who separately assessed the digital image and classified it as VIA-DCRC positive or negative.
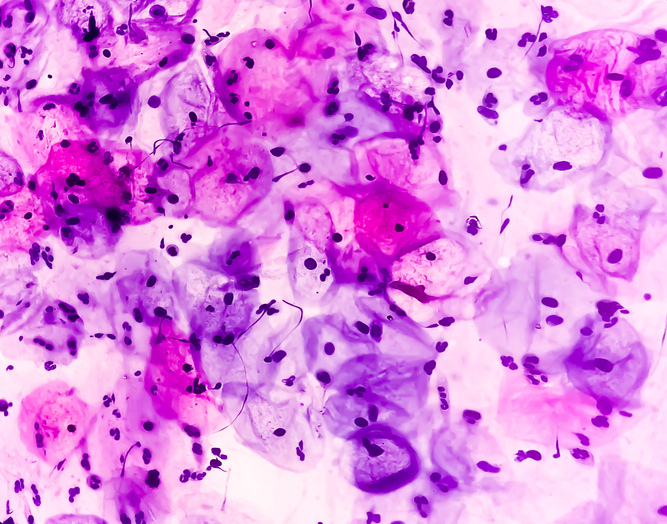
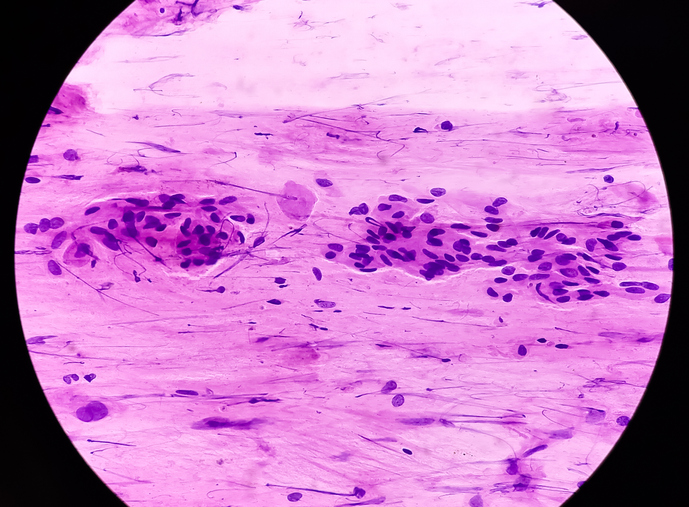
Any two opinions of the gynecologic oncologists that concurred were considered the final diagnosis. Measures of accuracy were estimated using the Bayesian method. All participants who screened positive for cervical cancer underwent colposcopy and biopsy prior to treatment. Tissue samples were obtained, and histopathologic examinations were performed.
The mean age was 39.7 ± 10.7 years. Average CD4+ count and plasma viral load (log base 10) were 492.2 cells/mm3 (standard deviation, 255.3) and 2.6 copies/mL (standard deviation, 0.7), respectively. Overall, 60.5% participants were diagnosed with cervical precancer (VIA, 23.1%; 95% CI, 10.1-37.5; VIA-DCRC, 37.5%; 95% CI, 26.6-50.1).
“Cervical cancer screening in HIV + women using VIA/DCRC is feasible and it significantly improves the sensitivity, and comparable negative predictive value of VIA in diagnosing the presence of cervical pre-malignancies by more than double, and 65% respectively,” the researchers concluded.
Source


 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.