Pembrolizumab plus chemoradiotherapy was shown to improve survival in newly diagnosed patients with high-risk, locally advanced cervical cancer (CC), according to a randomized, phase III (ENGOT-cx11/GOG-3047/KEYNOTE-A18) clinical trial published in The Lancet.
Progression-free survival (PFS) was measured in the first interim analysis of the study, at which point Domenica Lorusso, MD, PhD, and colleagues found that the treatment combination resulted in a “statistically significant and clinically meaningful improvement” among patients.
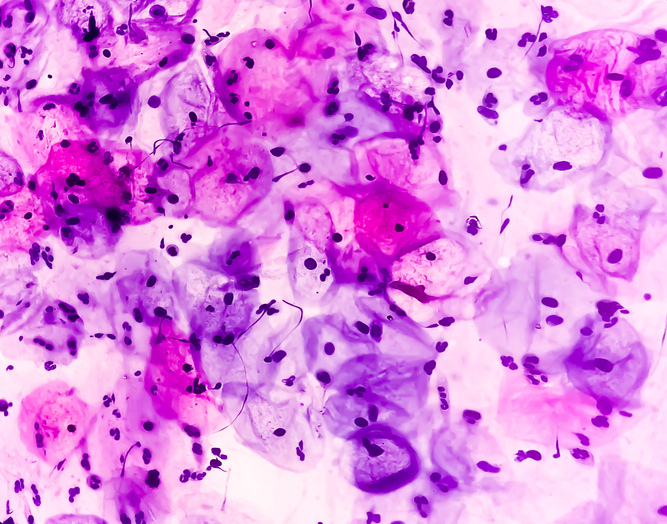
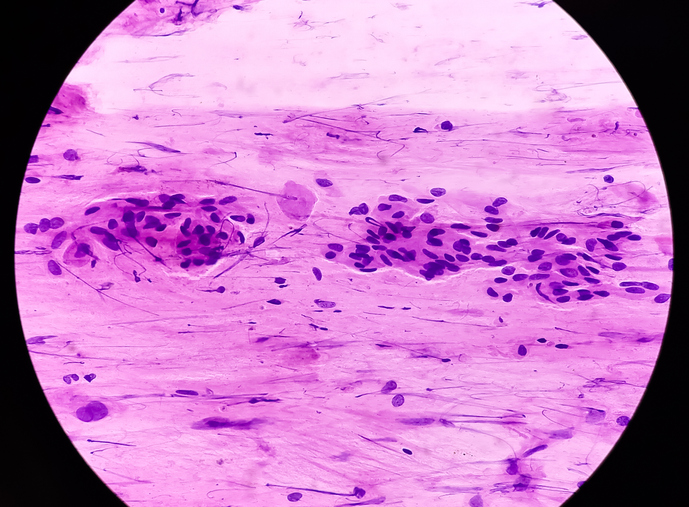
In the second interim study analysis, eligible participants, patients with newly diagnosed, high-risk, (FIGO 2014 stage IB2-IIB with node-positive disease or stage III-IVA regardless of nodal status) adenocarcinoma, squamous cell carcinoma, or adenosquamous CC, were assessed for overall survival (OS) by Dr. Lorusso and colleagues. OS was defined as the time from randomization to death due to any cause.
Upon randomization, patients were divided by cancer stage at screening, planned total radiotherapy dose, and planned external beam radiotherapy type. 1,060 patients across 30 countries were intravenously administered at random placebo or five cycles of pembrolizumab (200 mg) every three weeks, in addition to chemoradiotherapy, followed by 15 cycles of placebo or pembrolizumab (400 mg) every six weeks. 531 patients were in the placebo-chemotherapy cohort and 529 patients were in the pembrolizumab-chemoradiotherapy cohort.
According to the results, the 36-month OS was 74.8% (70.1-78.8) in the placebo-chemoradiotherapy group and 82.6% (95% CI 78.4-86.1) in the pembrolizumab-chemoradiotherapy group. The median OS was not reached in either group and the median follow-up for both groups was 29.9 months (interquartile range [IQR] 23.3-34.3). 371 (70%) out of 530 individuals in the placebo cohort experienced a grade 3 or higher adverse event compared to 413 (78%) out of 528 patients in the pembrolizumab cohort. The most common adverse events were decreased white blood cell count, anemia, and decreased neutrophil count, and potentially immune-mediated adverse events were observed in 90 (17%) out of 530 patients versus 206 (39%) out of 528 patients in the placebo and pembrolizumab groups, respectively. The hazard ratio for death was 0.67 (95% CI 0.50-0.90; P=.0040).
“These data, together with results from the first interim analysis, support this immune-chemoradiotherapy strategy as a new standard of care for this population,” the researchers concluded.


 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.