Researchers from the Karolinska Institutet and Queen Mary University of London conducted a post hoc study on a trial that included 855 women in England who had a positive HPV test result, indicative of human papilloma virus (HPV) infection, in a self-collected vaginal tissue sample (self-sample) and a subsequent positive result on a sample obtained by a clinician. It was found that 71 of these women (8.4%) had severe cervical precancer or cancer. Results were published in PLOS Medicine.
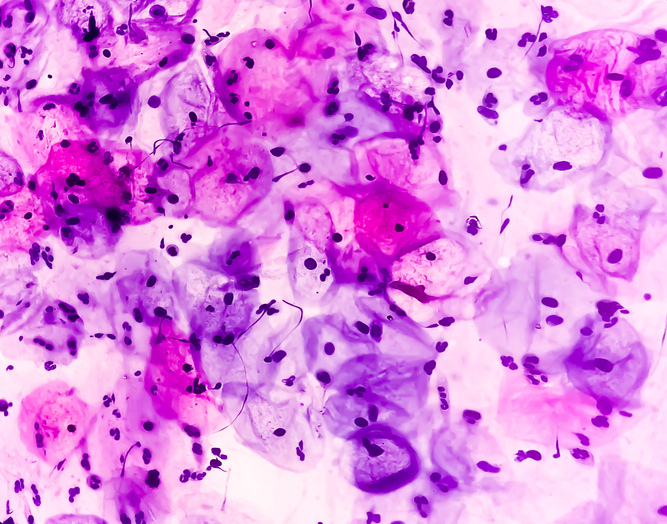
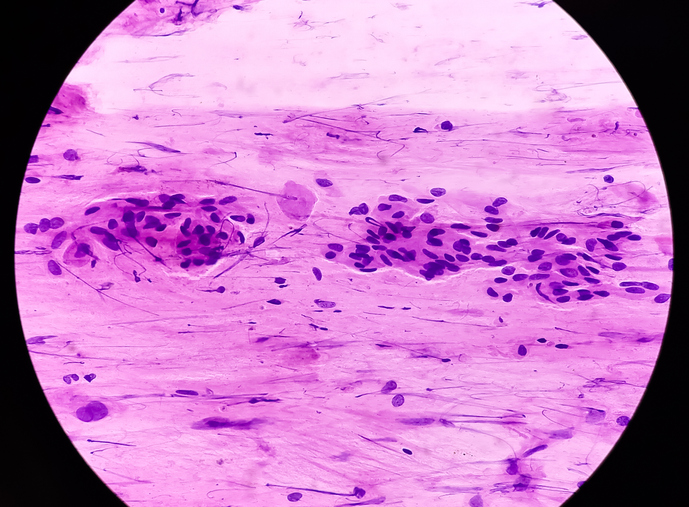
The researchers looked at the details of the HPV test results in self-samples and used a new method to assess the risk for severe cellular changes. They used a stratification approach, based on the variant of HPV and the amount of virus (measured as the cycle threshold [Ct] value) present in the self-sample; they divided HPV-positive individuals into three distinct risk groups based on HPV Ct values and genotypes (HPV16, HPV18, or other high-risk type) from HPV-positive self-samples.
The researchers classified 5% (44 of 855) of the individuals (HPV-16 Ct < 30) who tested positive for HPV on their self-collected sample as high risk, with 43.2% (19 of 44) of them having CIN2+, which is comparable to those with HPV-positive and abnormal cytology results who are referred for colposcopy in England. The low-risk group (HPV non-16/18 Ct ≥ 30), comprising half of those with HPV detected in a self-sample, has a risk of CIN2+ of 4.0% (18 of 452), which is lower than in those who are positive for HPV but have normal cytology findings on routine screening by a clinician.
“The proposed classifier allows those at greatest risk (high-risk group) to be sent directly to colposcopy and detects 3 quarters of CIN2+ without delay while allowing half of individuals (low-risk group) to be managed by repeat self-sampling. The intermediate risk group could be referred to their general practises for clinical sampling. Findings support the potential use of this risk classifier in the management of HPV–positive self-samples within organised cervical screening programmes,” the researchers concluded.
Source


 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.