Greetings, DocWire News readers. I attempt here to summarize the most important updates from the 2021 International Myeloma Workshop (IMW) meeting. I will try to present information in a way free from hype. I do acknowledge my own biases, however – I am much more interested in clinical studies, even though there are amazing basic science scientists diligently working against this disease. In this update I will try to focus on updates that influence (or may influence) my clinical practice, or that are very thought- provoking and novel.
1. The MASTER Trial
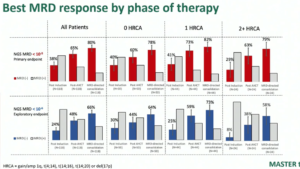
One can debate whether minimal residual disease (MRD) is a true surrogate of survival, or just prognostic (which is what I think the data currently show). However, as a proof of concept, the MASTER trial is MRD done right.
In this trial, newly diagnosed patients with myeloma received 4 cycles of induction with Dara-KRD (daratumumab with carfilzomib, lenalidomide and dexamethasone), followed by stem cell transplant, followed by consolidation with Dara-KRD, followed by lenalidomide maintenance. Patients who achieved MRD negativity after either transplant, or either 4 or 8 cycles of consolidation with Dara-KRD could be placed on treatment free observation (and forego additional consolidation or maintenance).
A total of 123 patients have been enrolled so far with a median follow-up of close to 2 years. High risk patients (57% had at least one high risk feature) and racial minorities (21%) were well represented. There were 2 unwitnessed sudden deaths on treatment (!!), but overall no surprising adverse events.
With the primary endpoint of 10-5, 80% of patients reached MRD negativity after MRD directed consolidation with Dara-KRD, and 66% of patients reached 10-6. Patients with 2 or more high risk features had slightly lower rates of deeper MRD negativity (58% reached 10-6).
As a proof of concept, this shines. However, 6 patients still progressed while on therapy, all displaying chromosome 1q gain (Gain1q), which speaks to the difficulty of treating Gain1q disease appropriately. This is still a small study, albeit one where a conscious effort made to recruit a diverse patient set. Long term follow-up will be very revealing. How are the patients at relapse treated? How durable are responses? How do we treat MRD positivity resurgence? Is it worth the toxicity and cost to treat asymptomatic MRD positive resurgent patients with aggressive therapy, just to obtain MRD negativity? Is this cost-effective in other resource settings? I am, however, a fan of the concept of using MRD to take off treatment, and the concept of this trial.
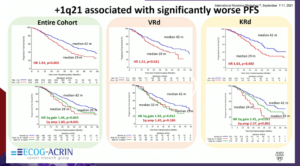
2. Post-Hoc Analysis of ENDURANCE (KRD versus VRD) with Respect to 1q Disease
So about 1q…I won’t spend too much time on this, since this post-hoc analysis is hypothesis generating and not definitive- but it goes to show how Gain1q patients generally have poorer outcomes with standard therapy. Patients did worse, whether they got VRD (bortezomib, lenalidomide, and dexamethasone) or KRD, although those who see merit in KRD for high-risk (which is a contentious topic) will say those with Gain1q had superior overall survival (OS) with KRD compared to VRD. Counterpoint – although not statistically significant, those with amplification of 1q (Amp1q) had BETTER OS with VRD compared to KRD. Really hard to make definitive conclusions, but in general, 1q is a tough patient population to treat.
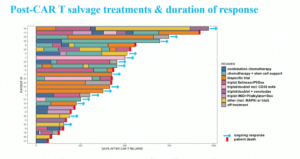
3. Trajectory of Patients Post-CAR T Relapse
There is life after CAR T (chimeric antigen receptor T cell therapy). In an analysis of 31 patients from Mt. Sinai who relapsed post CAR T, the median progression-free survival (PFS) was 3 months and OS was 15 months. This in a way reaffirms that the patients who make it to CAR T are in many ways a selected lot: “biologically” as well as in terms of access to care. These patients received a variety of treatment regimens (responses to bispecific CAR T in particular were often relatively durable), but even selinexor plus a doublet occasionally led to a response greater than 3 months. Definitely thought provoking, and perhaps shows that with access to treatments, these patients can often continue to experience disease control.
4. Breaking Through the FORTE of High Risk?
The results of FORTE for high-risk chromosomal disease gets a lot of attention, especially as pertains to lenalidomide-carfilzomib maintenance following a stem cell transplant. In the second randomization of this trial, patients were randomized to either lenalidomide (R) maintenance or carfilzomib + lenalidomide (KR) maintenance.
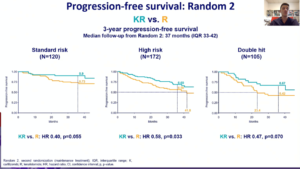
So, amongst the 172 high risk patients (now with 37 months of follow-up from second randomization), patients on KR maintenance continue to have a longer PFS than R maintenance. This lends credence to the argument of using doublet maintenance incorporating a proteasome inhibitor (PI) in patients with high-risk disease, which previously had been largely based on a cumulative interpretation/synthesis of older data demonstrating the superiority of bortezomib relative to thalidomide, and the relative lack of efficacy of lenalidomide maintenance in subset analysis of patients with high-risk disease .
I still struggle severely with PFS being used as the benchmark for maintenance. The onus has to be to show that outcomes are better (as in people live longer or better rather than just delaying progression) in this situation. However, the data has promise, and indeed will reaffirm the myeloma community’s decision to use doublet maintenance following a transplant for high-risk disease.
5. Cilta-cel Used Early: Preliminary Results from CARTITUDE-2
In a preliminary analysis of 20 patients with 1 to 3 prior lines of therapy who received the CAR T ciltacabtagene autoleucel (cilta-cel), 19 of 20 patients responded with no progression observed with a median follow-up of 6 months.
Promising, but as a side note I remain very bothered by how cilta-cel is being compared to just VRD de-escalated to lenalidomide alone in a Phase III trial for newly diagnosed disease (CARTITUDE-5), that will largely end up enrolling patients who could/should have been transplanted. I mean, if someone if CAR T eligible, shouldn’t they usually also be transplant eligible? If we want to use this instead of transplant in newly diagnosed, let’s compare against transplant. However, that would take years to show, and I think the sponsors of the trial want the cheaper, easy route.
6. Updated Follow-Up of CARTITUDE 1
Cilta-cel continues to have durable responses for heavily relapsed disease. With a median follow-up of 18 months, amongst the 97 patients who actually received CAR T (remember this isn’t an intention to treat analysis!) a response rate of 98% and median duration of response of 21 months were seen. I still think the neurological issues need to be further categorized, as 5 patients did develop neurocognitive/motor changes, and these weren’t necessarily always reversible.
7. BiTEs Beyond Just BCMA
So, I am genuinely excited about the prospect of targeting non-BCMA (B cell maturation antigen) receptors with BiTEs (bispecific T cell engagers). Talequetamab targets GPRC5D, and this concept is exciting. The results are super preliminary, with only 30 patients dosed at the recommended phase 2 dose. Seventy percent of those patients responded, and at 6 months most patients had continued responses. It’s important to note that only 8 of these 30 patients had prior BCMA therapy, not all of them. We don’t know whether or not those patients responded, as that was not reported. Also, 60% of patients at recommended phase 2 dose experienced dysgeusia, which is unpleasant and is not a side effect to be minimized. However, the thought of targeting a receptor after BCMA holds a lot of promise!
8. An OCEAN of Failure
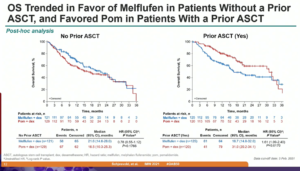
Unfortunately, melphalan flufenamide’s (melflufen) confirmatory Phase III confirmation trial (OCEAN) was quite disappointing. In this trial, melflufen plus dexamethasone (mel-dex) was compared to pomalidomide plus dexamethasone (pom-dex) in heavily pre-treated disease (2-4 prior lines of therapy).
In an intent to treat analysis of all patients, melflufen did narrowly meet the primary end-point of PFS (hazard ratio [HR]=0.77, 95% confidence interval [CI]; 0.63 to 0.95). However, melflufen failed on OS. In patients without prior autologous stem cell transplant (ASCT), melflufen had a non-significant improvement in OS (HR=0.78, 95% CI;0.55 to 1.12). However, in patients with a prior ASCT, there was a clinically and statistically significant decrement in OS (HR=1.61, 95% CI; 1.09 to 2.40). The difference in median survival was quite high for this patient population (31 months for pom-dex versus 16 months for mel-dex). If pom-dex was a new intervention, these results would have been a verdict celebrated by all the community.
Even though I have seen some statements following this presentation that claim that melflufen is a valid option in patients who have not received prior ASCT, this is very problematic for several reasons. In my opinion, melflufen is a solid reminder of how often extremely attractive basic science doesn’t translate to clinical results. Melflufen was sold to us from pre-clinical data as having the potential to reverse melphalan resistance and being significantly more potent and specific to cancer cells than previous alkylators. These results essentially demonstrate that the only patient population melflufen works safely and well in are the same patient populations who are expected to respond well to alkylators anyway: those who haven’t gotten a prior transplant.
We have zero clinical evidence that melflufen is any better or safer than oral melphalan or cyclophosphamide or bendamustine, and the confirmatory trial LIGHTHOUSE (which was comparing a triplet of daratumumab/melflufen/dexamethasone versus daratumumab monotherapy) wasn’t going to get us any closer to that answer. I also would like to know exactly how/why patients died, and that information was missing from the presentation. The comments during the Q/A session on melflufen being safe if transplant was in the remote past (more than 5 years ago) are far from definitive and need to be backed by solid prospective data.
Even though I have been harshly critical of selinexor in the past, there is still a unique niche for that drug today in certain heavily refractory populations. I really cannot say the same for melflufen. Melflufen can still carve out a path for itself in the following scenarios, 1) by comparing against a standard alkylator in heavily pre-treated disease, and 2) by showing it is safer and more/as effective than standard high-dose melphalan therapy when used at myeloablative doses.
Other Honorable Mentions
1. Whole body magnetic resonance imaging (MRI) or positron emission tomography/computed tomography (PET/CT)? In this intriguing analysis by Martin Kaiser (the iTIMM study), in a single center prospective observational study of 60 patients with myeloma intended for transplant, whole body MRI was more sensitive than PET/CT in detecting lesions. Very thought provoking, although I don’t know if I would fully pivot just yet. A philosophical question: Is there value to “detecting” additional lesions that are asymptomatic and don’t change management? This may be a more important consideration when a diagnosis of multiple myeloma versus smoldering myeloma is in question.
2. A link between diet consumption and outcomes in myeloma? Intriguing work by Dr. Shah from Sloan Kettering, although obviously very far from definitive. Thirty-four patients were able to fill in self-reported questionnaires about dietary intakes and provide stool samples, and increased plant and seafood protein intake was associated with higher stool butyrate levels which were in turn associated with higher rates of MRD negativity. Were the stool butyrate levels different because of a life-long history of healthy eating, good habits, higher socioeconomic status and medical compliance? Can intervening with a plant-based diet for a period of time change butyrate levels and actually change outcomes? This is hypothesis generating and much needed/fantastic work, but for now I will keep telling my patients to eat healthy but also eat whatever they love eating to maintain calories, as its tough enough already without imposing additional dietary restrictions.
3. Venous thromboembolism (VTE) in the GRIFFIN study? I echo my mentor Dr. Douglas Sborov’s thinking on this: More can be done to prevent VTE. In the GRIFFIN study, VTE occurred in 10% of patients treated with daratumumab plus VRD, and 15% of patients treated with VRD alone. This should be considered with the knowledge that retrospective data (and partial data from trials) suggests KRD has an even higher rate of VTE than VRD. In the ENDURANCE trial, only Grade III-V VTE was reported, and the rates were 5% versus 2%. Grade II VTE (i.e., an uncomplicated deep vein thrombosis) is essentially unknown from that study and it would be nice if that could be reported.
4. A low-cost way to check the M protein? Work utilizing MALDI-TOF mass spectrometry by Dr. Nikita Mehra deserves a mention. This represents amazing low-cost, indigenous technology from India that detects the M protein with very high concordance rates with traditional serum protein electrophoresis (SPEP).
Dr. Ghulam (Manni) Mohyuddin is Assistant Professor in the Division of Hematology and Hematologic Malignancies at the University of Utah School of Medicine. Dr. Mohyuddin specializes in hematological malignancies and multiple myeloma, and is currently completing a fellowship with research interests that include racial disparities, drug repurposing, quality of scientific methods, end-of-life care, cost-effectiveness and evidence-based care, and medical education. He has published in more than 39 peer-reviewed publications. Follow Dr. Mohyuddin on Twitter @ManniMD1.
Visit DocWire’s Multiple Myeloma Knowledge Hub here.







 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.