The Role of Multidisciplinary Care in Head and Neck Cancer
By Eric Bergson, MD, Rob Dillard - Last Updated: April 24, 2025April is Head and Neck Cancer Awareness Month. Oral, Head, and Neck Cancer is a common type of cancer worldwide, with around 650,000 new cases diagnosed each year. Factors such as tobacco use, excessive alcohol consumption, poor diet, and exposure to the human papillomavirus can increase the risk of developing this type of cancer.
“Many cancers produce early warning signs. Oral, head, and neck cancers are no different and produce symptoms that when detected early enable physicians to successfully treat the cancer,” says Eric Bergson, MD, an otolaryngologist and head and neck surgeon with ENT and Allergy Associates in Suffolk County, NY, “Early detection is the best defense in successfully treating head and neck cancers—it allows for prompt treatment and better outcomes. Knowing the symptoms and warning signs gives you the knowledge you need so that you can alert your physicians as soon as possible.”
DocWire News spoke with Dr. Bergson about the importance of head and neck cancer awareness, how to integrate screening into routine patient care, and the role multidisciplinary collaboration plays in managing head and neck cancer.
Transcript:
DocWire News: What are the most common early signs and symptoms of head and neck cancers that physicians should be vigilant about during routine examinations?
Head and neck cancer is a broad topic that includes many different things, but if I were going to bring one thing to the forefront, it would be a mass or a lump in the neck. So, the patient was shaving, and they said, “Oh, what’s this lump that I feel in my neck?” A neck mass or lump, they notice, is probably the number one presenting symptom.
How can physicians integrate screening for head and neck cancers into routine care, especially for high-risk populations such as smokers or those with HPV exposure?
Well, that’s a good question. It has a lot of different aspects. A primary care physician will do a basic physical exam. They’re going to look in the mouth, they’re going to feel, and examine the neck with palpation. We might look closer in the ENT office, possibly using a flexible laryngoscope. But the idea of the risk stuff is tricky, really, honestly, it is. Certainly, smoking and drinking are going to be big risk factors, but those are very much on the decline.
You brought up HPV. HPV is a new form of head and neck cancer, and there are no risk factors. Most adults who have had an average, let’s say, sexual life, most adults who were not in monogamous relationships from junior high on have been exposed to HPV. That’s just the reality; It’s a ubiquitous exposure that is a function of the host immune response. Some of these conversations could be a little tricky, but it’s not like you’ll start probing people’s history and finding out who’s at risk and who’s not. You have to assume that the risk is just ubiquitous.
The head and neck cancer aspect is quite a bit more common in men than women. I’m not sure there’s a known cause for that. In the decades to come, we should see a precipitous decline in it because the HPV vaccinations that the younger generation receives are enormously effective for cervical cancer in women. It appears that it should be just as effective in preventing head and neck cancer. So that’s why adolescents, it’s recommended that they get it prior to the onset of sexual activity, so that they can be protected. It should be a cancer that it shouldn’t happen. I mean, anything’s possible, and I’ve heard circumstances where it evades it, but the HPV vaccines are tremendously preventative.
With advancements in treatment, how do physicians assess the balance between preserving function (e.g., speech, swallowing) and effectively treating head and neck cancers?
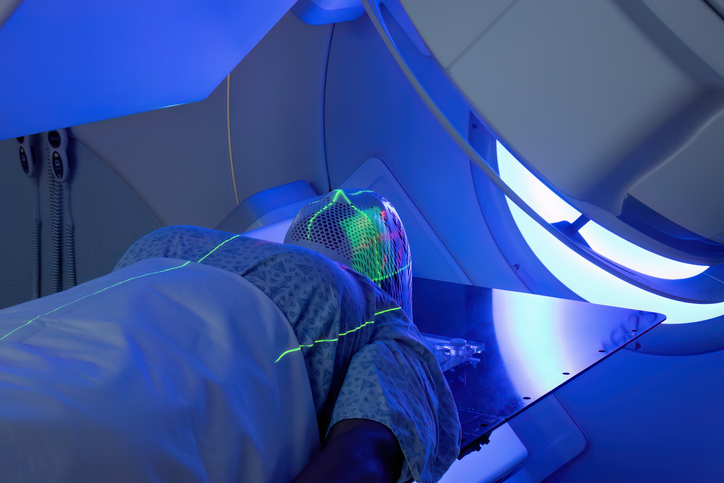
The treatment options end up being some combination of surgery, radiation, and chemotherapy. It’s a balance. It’s a question of preserving function and eradicating the tumor. Every situation is different. The different tumor stages lend themselves to different options, right? An earlier stage situation may lend itself to surgery alone. If you can have surgery alone, you avoid the side effects of radiation on the delicate tissues of the throat. But sometimes there’s too much to remove, and you end up sacrificing function, and that’s where sometimes the radiation and the chemotherapy become better options. There’s only so much tissue in the back of the throat; there’s only so much tissue in the back of the tongue that you can remove without causing a functional deficit. I’m not sure I can provide a definitive answer, but I can say that it’s an important part of the decision-making process for what’s going to be the best treatment for each person’s individual tumor.
What role does multidisciplinary collaboration (e.g., with oncologists, surgeons, speech pathologists) play in the management of head and neck cancer, and how can physicians better coordinate care for these patients?
The term you’ll hear is multidisciplinary care, and that’s what it is. In a perfect world, you have what are called tumor conferences, which are often over Zoom in today’s day and age, with surgeons, radiation oncologists, and medical oncologists discussing patient care. There’s often a perception that treatment is completely standardized and there’s a right treatment and a wrong treatment, but it’s really unclear. There’s a lot of judgment, and then there are different opinions and options.
Each specialty brings its own experience to the conversation. One person might say, “Oh yeah, I thought this was a good person to just have surgery,” and the surgeon might say, “Yeah, but did you look at how close it is to such and such? I don’t know that I can get that out safely.” Non-surgeons may not appreciate that aspect. You have these different specialists in a room, a virtual room usually at this point, going through the discussion of the other cases, offering different opinions until a consensus is reached about how best to handle it.
That’s a perfect world. If you can’t engage in a tumor conference, you can do the next best thing: have various physicians you may interact with and talk to. So you don’t have a tumor conference, but you can call your colleague, the radiation oncologist, and say, “Hey, I want you to see this guy. I don’t think it’s a great surgical candidate. Why don’t you take a look, see what you think?” That kind of conversation is always going to be the best way. The tumor conference is nice because it puts everybody in the room simultaneously to conduct an active discussion, but not everybody has access to that situation. As long as you try to collaborate with your colleagues, you can accomplish most of the same things.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.