
There is a positive association between melanoma and Parkinson’s disease (PD), with the risk for melanoma ranging between 1.4- and 20-fold among individuals with PD. The risk is bidirectional, too, because there is also a 1.7- to 4.2-fold increased risk for PD in patients with melanoma. The link between PD and melanoma is not well understood, but increased expression of the PD-associated protein alpha-synuclein (αSyn) in melanoma cells may provide insight into the positive association between the two diseases.
Researchers tested the function of αSyn within melanoma cell nuclei to better understand the link between neurodegeneration and cancer. The results were published in Science Advances.
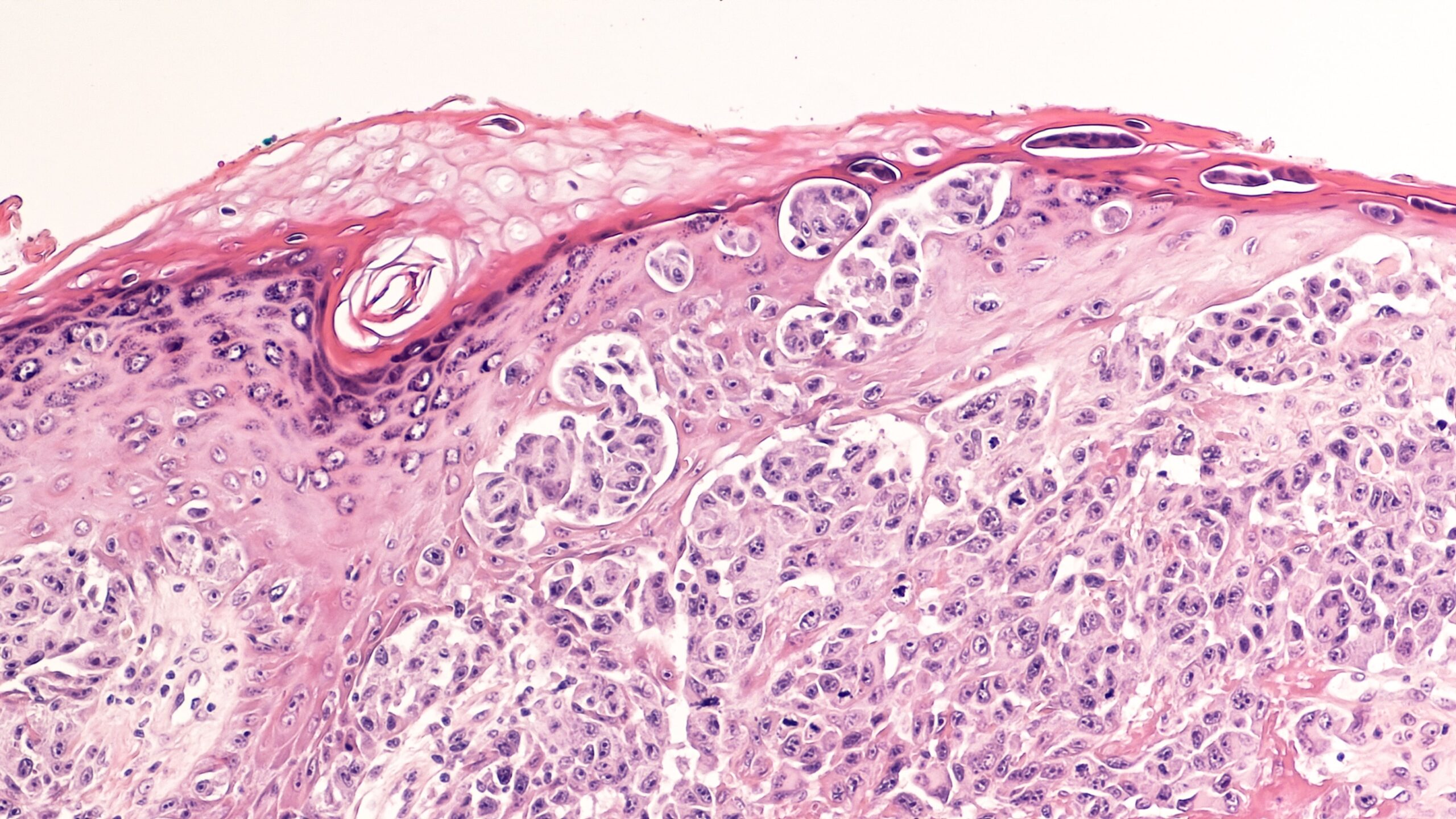
The researchers tested the spatial pattern of αSyn within primary cutaneous melanoma cells (n=4) and brain metastatic melanoma (n=17). Four out of 4 and 15 out of 17 cells demonstrated αSyn staining; immunofluorescence staining revealed a clear enrichment of αSyn near the large replication protein A2 (RPA32) foci, which resemble nucleolar structures involved in ribosomal DNA (rDNA) double-strand break (DSB) repair.
Further staining of primary and immortalized melanocyte and melanoma cell lines showed consistent nucleolar localization of αSyn across nearly all cells. In the SK-Mel28 melanoma line, αSyn was found in 4’6-diamidino-2-phenylindole (DAPI)-poor regions and colocalized with known nucleolar markers: treacle, nucleophosmin, and nucleostemin. Similar patterns were observed in A375 (melanoma), PIG1 (melanocyte), and primary human melanocytes.
Using fluorescence deconvolution, the researchers examined αSyn localization within nucleolar subcompartments, specifically the fibrillar center (FC), dense fibrillar component (DFC), and granular component (GC). Antibody staining specific to each compartment (RPA194 for FC, fibrillarin for DFC, and nucleophosmin for GC), along with 3D reconstruction, revealed that αSyn is mainly localized to the GC, adjacent to the DFC, and largely excluded from the FC.
This was further validated through immunogold transmission electron microscopy, which showed αSyn labeling concentrated in the GC and/or DFC, but not the FC. Labeling was significantly reduced in αSyn knockout SK-Mel28 cells. These findings indicate that αSyn is localized within the nucleolus of melanocytes and melanoma cells, with a strong preference for the GC region.
To explore the functional role of α-synuclein (αSyn) in the nucleolus, researchers assessed levels of γH2AX, a marker for DNA DSB repair, in both the nucleoplasm and nucleolus. They found that both αSyn and γH2AX were significantly more abundant in the nucleolus, with strong colocalization in SK-Mel28 cells and in PIG1 and primary melanocytes. Proximity ligation assays confirmed that αSyn and γH2AX are closely associated within DSB repair foci.
In αSyn knockout cells, γH2AX levels were elevated, particularly in the nucleolus, suggesting that αSyn plays a more critical role in DSB repair within the nucleolus than in the general nucleus. Reintroducing wild-type αSyn into knockout cells restored γH2AX levels to normal. These findings were corroborated by Western blot analysis following nuclear fractionation.
“This could lead to deficient DSB repair that contributes to programmed cell death,” the researchers noted.
“Our current data suggest that these same individuals could also be predisposed to develop melanoma via a gain-of-function mechanism where increased αSyn levels improve DSB repair capacity within the nucleolus, which limits the senescence and programmed cell death pathways that are triggered by excessive DSBs associated with oncogenesis. This provides a framework for understanding the link between PD and melanoma and offers potential therapeutic targets in melanoma that are focused on reducing αSyn-mediated nucleolar DSB repair,” they concluded.
Reference
Arnold MR, et al. Sci Adv. 2025;11(15):eadq2519. doi:10.1126/sciadv.adq2519




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.