A research team from the Cold Spring Harbor Laboratory in New York have recently identified two cell mutations that work in concert to enhance the development of acute myeloid leukemia (AML). These two mutations are already harmful on their own, but according to this new CSHL study, their effects in AML are exacerbated when both are present. This work was published on October 2 in the journal Nature.
Alongside Omar Abdel-Wahab at Memorial Sloan Kettering Cancer Center, CSHL Professor Adrian Krainer and his lab identified how mutations in the IDH2 and SRSF2 genes team up to cause AML. Mutations in IDH2 appear to enhance errors that are caused by the SRSF2 mutation, which prevents bone marrow cells from maturing into red and white blood cells in AML sufferers with these mutations. Currently, Krainer and colleagues are working to target this genetic cooperation in treating this aggressive blood cancer.
“This all started when we were looking at patient data in The Cancer Genome Atlas and saw that again and again deadly cases of AML had both these mutations,” explained Abdel-Wahab, a hematologist oncologist.
These two mutations are known for their involvement with symptoms that precede cancer, but their definitive contribution to cancer was not known before this work. Abdel-Wahab and Krainer teamed up to identify how IDH2 and SRSF2 function together in AML.
“Just because you see a mutation [in a sick patient’s cells] doesn’t really show that it’s directly contributing to the disease,” said Krainer.
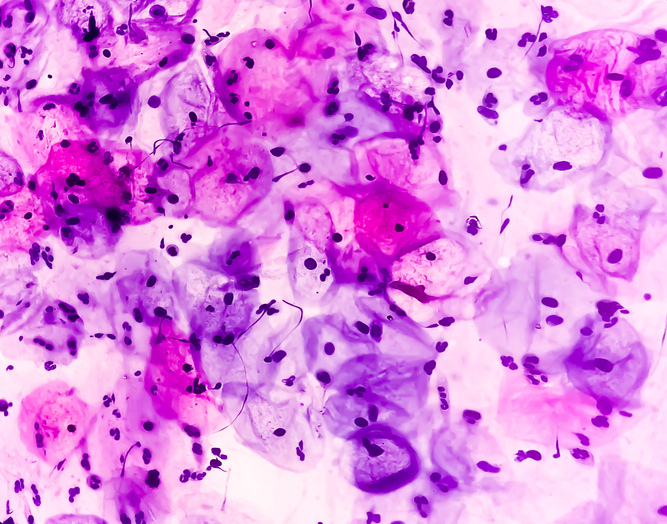
Prior to their work, research has found that a mutated SRSF2 gene can cause errors in the RNA splicing process, which is essential in the transition from DNA code to tangible protein products. Faulty RNA splicing can cause significant detriment to one’s ability to express genes properly.
Being that DNA tests initially found SRSF2 mutations in only 1% of AML patients, researchers did not think that the splicing deficiency caused by the mutation was tied to the disease. Krainer’s lab found that this issue is much more common than this, however, affecting roughly 11% of AML patients. This discovery was made by Kuan-Ting Lin, a postdoctoral researcher in Krainer’s lab, who was searching for the SRSF2 mutation in RNA rather than DNA.
“Dr. Lin is very patient, looking at massive amounts of data and picking up distinct patterns and making connections between things that aren’t obvious to everyone,” noted Krainer.
Building on this information, Abdel-Wahab’s lab found that the splicing errors caused by SRSF2 are enhanced when a mutation in IDH2 is present. This results in a higher number of defective blood cells, and in turn, worsened AML.
“So in some ways, these two genes, when defective, are cooperating,” explained Krainer. “Now that we do know about this interdependence, we may find points where we can intervene.”
Mutant cells team up to make an even deadlier blood cancer, scientists at Cold Spring Harbor Laboratory have discovered https://t.co/8FthPTM4Gs via @medical_xpress
— delthia ricks ? (@DelthiaRicks) October 2, 2019





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.