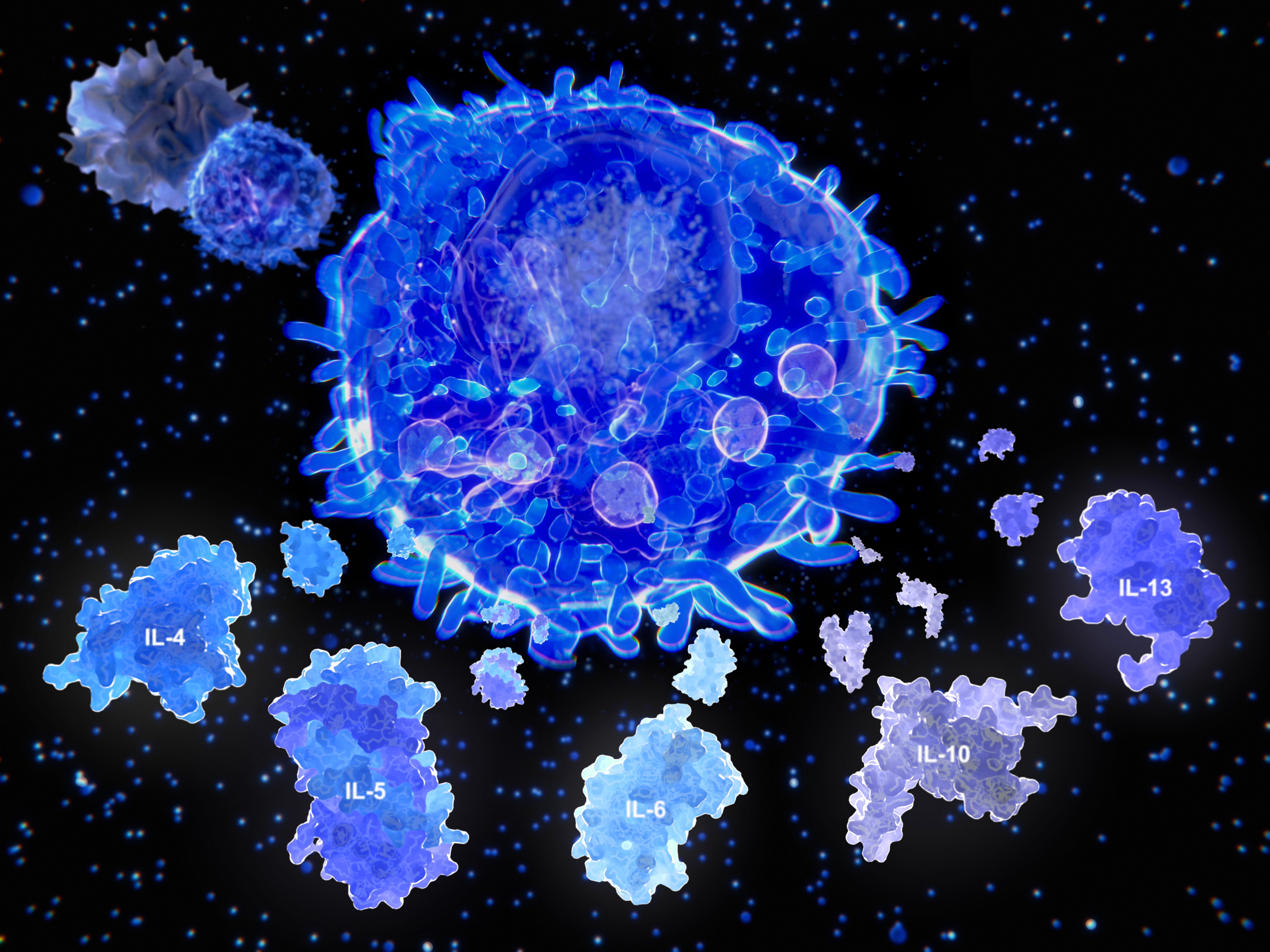
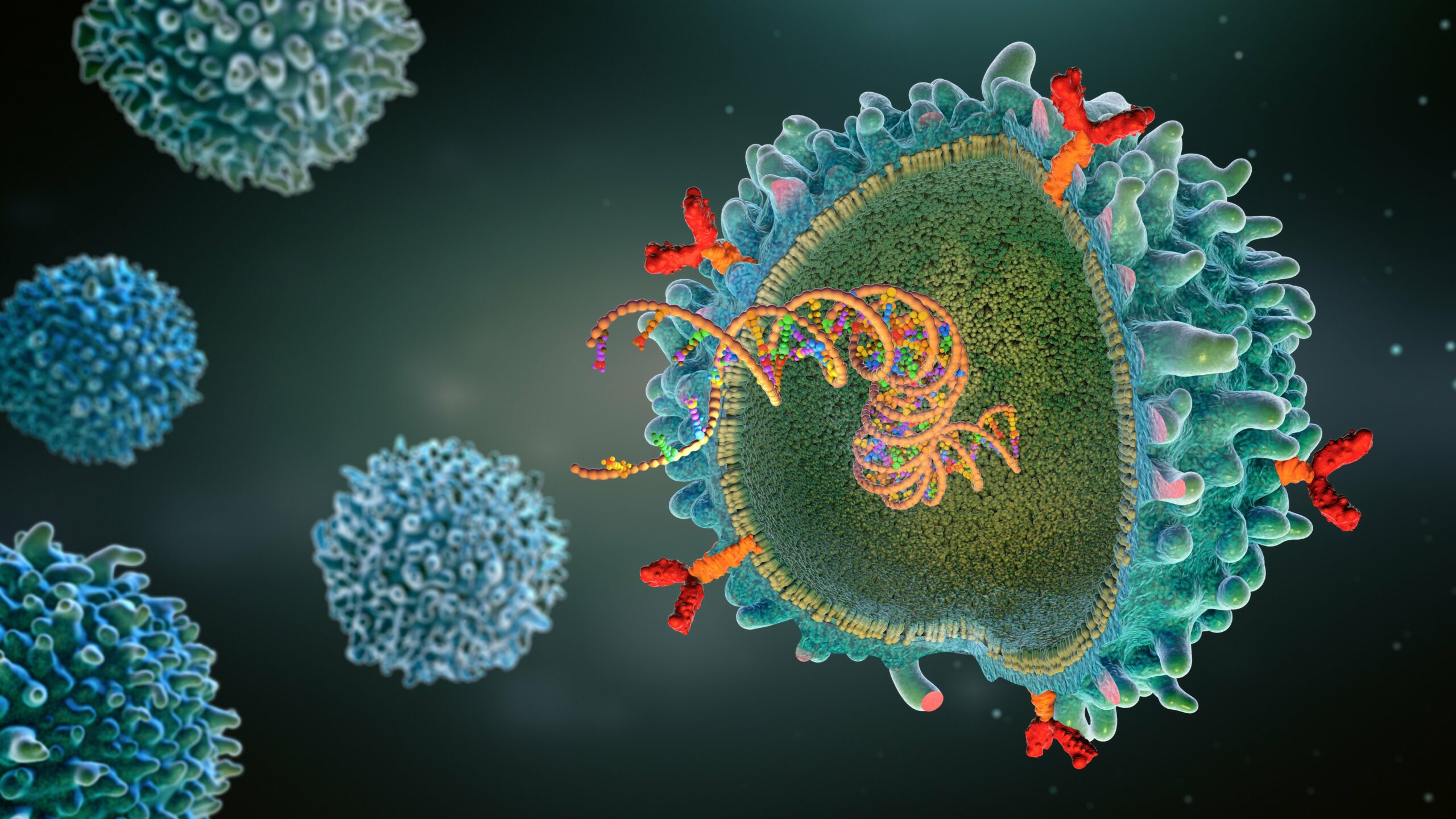
In patients with malignant hematologic neoplasms, cytokine storm (CS) can be initiated by many different causes. Among these are malignant neoplasm–associated hemophagocytic lymphohistiocytosis (MN-HLH), COVID-19 infection, and chimeric antigen receptor (CAR) T-cell therapy. A multidepartmental team of investigators from the University of Texas MD Anderson Cancer Center, Houston, conducted a study to see whether cases of CS outcomes vary by etiology.1
“Understanding the unique and shared features of CS etiologies may inform personalized treatment strategies, highlighting the importance of early diagnosis and targeted interventions for improving patient outcomes,” wrote first author James Long, PhD, of the Department of Biostatistics at MD Anderson, and colleagues. The investigators published their findings in JAMA Network Open.1
Their single-center retrospective cohort study enrolled 671 patients with malignant hematologic neoplasms who had experienced CS. Cytokine storm was initiated by COVID-19 infection in 34% of the patients, MN-HLH in 33%, and CAR T-cell therapy in 33%. The investigators noted that patients with CS initiated by MN-HLN had a significantly younger median age than patients with the other 2 initiators, at 55 years versus 63 years in both the COVID-19 and CAR T-cell therapy cohorts (P<0.001). They also noted that the patients in the 3 etiology cohorts differed in their underlying cancer types and number of admission days.1
The investigators found differences across the 3 etiology categories in patient inflammatory markers and survival outcomes. Patients with CS associated with MN-HLH had the highest levels of tumor necrosis factor-α, at 105 pg/mL versus 23 pg/mL in those with COVID-19 infection–linked cytokine storm, and the lowest fibrinogen and albumin levels. Cytokine storm linked to CAR T-cell therapy carried significantly longer survival time as compared with that linked to COVID-19 infection or MN-HLH, with hazard ratios of 2.93 and 8.12, respectively.1
From their findings and clustering analysis, the investigators concluded that CS episodes initiated by COVID-19 or CAR T-cell therapy shared certain inflammatory patterns that made them distinct from MN-HLH–based CS. MN-HLH–based CS also differentiated itself from CS of the other 2 etiologies by having worse survival rates.1
“The CAR-T–treated group exhibited the highest survival outcomes compared with the cohorts with COVID-CS [COVID-19 infection–initiated CS] and MN-HLH. Additionally, the findings suggest that CAR-T CRS [cytokine release syndrome] and COVID-CS share similar cytokine activation pathways, while MN-HLH operates differently,” wrote Long and colleagues in their conclusion.1
These findings published in JAMA Network Open were accompanied by an invited commentary from Andre C. Kalil, MD, MPH, Anum Abbas, MD, and Sias J. Scherger, MD, from the University of Nebraska Medical Center, Omaha.
The commentary authors pointed out that the findings from the CS etiology study have limitations due to the study’s retrospective nature and that to assess the generalizability of these findings, they will need to be replicated among patients in external hospital settings. However, the commentators praised the overall design of the study, especially the use of clustering techniques in combination with traditional statistical regression models, and highlighted that the study results were consistent even after adjustments for patient age, gender, and race.2
A current clinical need stressed by the commentators is for more awareness of the important differences there are among CS cases that are linked to the 3 etiologies. According to the commentators, the study by Long and colleagues1 gives an important practical contribution to this awareness, aiding clinicians’ ability to tailor management.2
“The new findings make a substantial contribution to our knowledge because now we have better means to understand patients’ inflammatory and coagulation profiles related to these 3 specific clinical syndromes. Regarding clinical practice, this study provides a more precise approach for health care practitioners to prognosticate and communicate with patients experiencing these clinical syndromes,” wrote the commentators.2
Reference
- Long JP, Prakash R, Edelkamp P Jr, et al. Cytokine storms in COVID-19, hemophagocytic lymphohistiocytosis, and CAR-T therapy. JAMA Netw Open. 2025;8(4):e253455. doi:10.1001/jamanetworkopen.2025.3455
- Kalil AC, Abbas A, Scherger SJ. Are all cytokine storms born equal? JAMA Netw Open. 2025;8(4):e253466. doi:10.1001/jamanetworkopen.2025.3466




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.