
Correspondence in the New England Journal of Medicine suggests that there has been a dramatic decline in stroke evaluations in the wake of the COVID-19.
A Letter to the Editor by a group of physicians from Stanford University and the Washington University School of Medicine laid out an analysis of a neuroimaging database that suggested a decrease of nearly 40% in stroke evaluation since the pandemic began.
“The effect of the COVID-19 pandemic on medical care for conditions other than COVID-19 has been difficult to quantify,” they wrote in the letter. “Any decrease in care for patients with acute conditions such as ischemic stroke may be consequential because timely treatment may decrease the incidence of disability.”
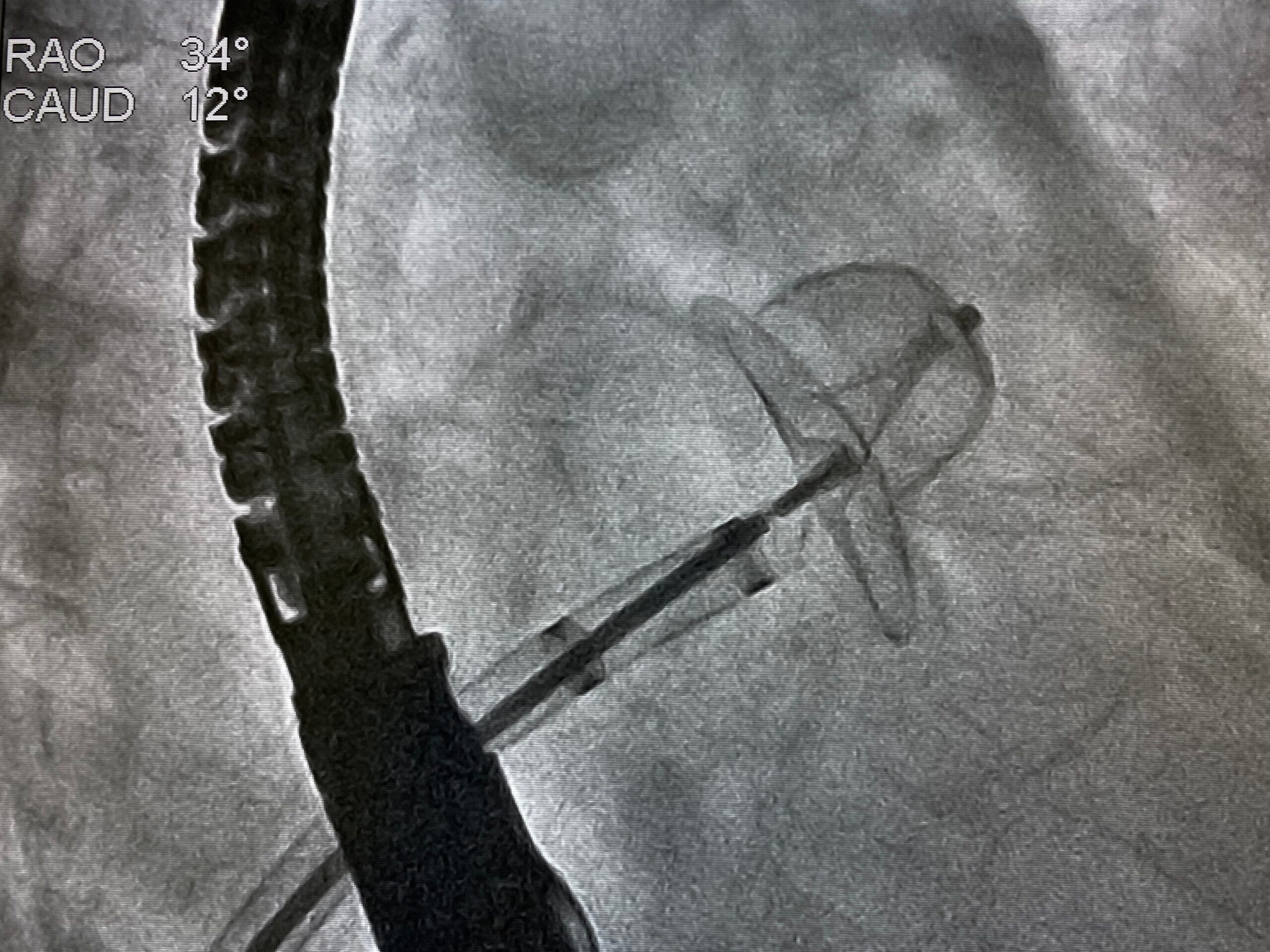
The authors used the RAPID software platform, which is typically used to gather data on patients that could potentially benefit from endovascular thrombectomy, were uploaded to a real-time data repository as a surrogate for the quantity of care provided by hospitals to patients with acute ischemic stroke. The analysis included data on more than 231,000 patients who underwent the imaging using the software in more than 850 hospitals in the United States between July 1 2019 and April 27, 2020. The authors compared the mean daily counts of hospital patients in the RAPID system in a 29-day period between February 1 and February 29, 2020 with mean counts during a 14-day period between March 26, 2020 and April 8, 2020.
[do_widget id=mashup_multiwidget-29]
The authors reported that the low point of daily counts occured during the 14-day period between March and April, decreasing by 39% from 1.18 patients per day per hospital in the pre-pandemic period to 0.72 patients per day per hospital during the early pandemic period. The decreases were seen across all age, sex, and stroke severity subgroups, suggesting decreases in the number of evaluations in both those with severe strokes as well as in nonelderly patients with low risk for COVID-19 complications. Regional differences were ruled out as a primary cause for the decreased use.
The use of the surrogate data for the care provided was cited as a limitation of the analysis.
“Across the board, everybody is affected by this decrease,” said Akash Kansagra, MD, assistant professor of radiology and neurology at Washington University’s Mallinckrodt Institute of Radiology, and the lead author of the analysis, said in a news release. “It is not limited to just hospitals in urban settings or rural communities, small hospitals or large hospitals. It is not just the old or the young or the people with minor strokes who aren’t showing up. Even patients with really severe strokes are seeking care at reduced rates. This is a widespread and very scary phenomenon.”






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.