
Overview of Minimal Residual Disease
Minimal residual disease (MRD) is the small number of cancer cells that can remain in a patient’s body after treatment and during clinical remission (CR) that may be an early indicator of relapse and disease recurrence.1,2 Both positive and negative MRD status may be used to inform treatment choice, assess response to therapeutic intervention, and predict long-term clinical outcomes.3
MRD can be detected through testing with a variety of assessment tools – each of which has unique sensitivity, standardization, sample requirements, turnaround time, and availability:
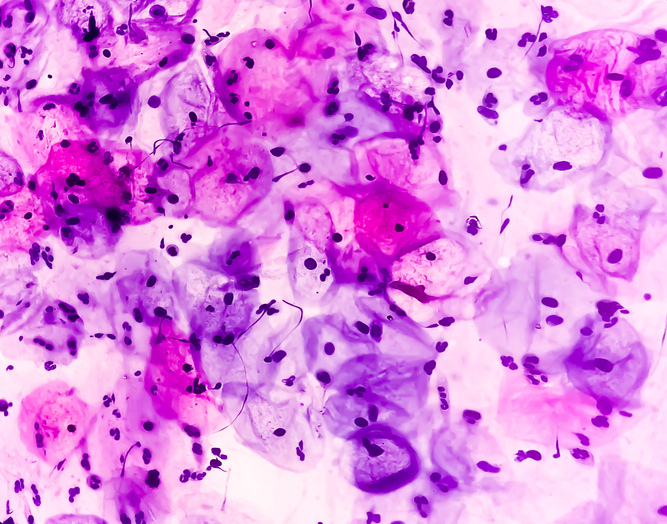
- Light microscopy has been in use for more than a century but is not as sensitive in detecting lower levels of MRD, compared with newer technologies.4-5 Microscopy has an approximate sensitivity level of 5 percent.6
- Flow cytometry fluorescently labels cells with abnormal surface markers associated with leukemia and multiple myeloma (MM) and counts them via laser.7,8 This method has a sensitivity level of approximately 0.01 percent.9 The EuroFlow consortium, however, has developed a test with a sensitivity level of up to 0.002 percent. Flow cytometry is subject to laboratory variability based on the operator and equipment used, making it a difficult method to standardize.10
- Polymerase chain reaction (PCR) identifies gene rearrangements specific to a patient’s diagnosis and creates custom primers to detect and quantify their presence.7,11 PCR has a sensitivity level of up to 0.001 percent, but because the primers are patient-specific, this method can be time consuming and cannot be standardized.6,12
- Next-generation sequencing (NGS) is the newest method of MRD assessment. It uses DNA sequencing technology to characterize and quantify B- and T-cell receptors from a single patient sample.13,14 The sensitivity of NGS consistently approaches 0.0001 percent; the assay is not as locally available as flow cytometry but is considered easier to standardize.15
The use of MRD status was incorporated into recent U.S. Food and Drug Administration (FDA) approvals: In 2018, blinatumomab became the first and only FDA-approved MRD-directed therapy, with an indication for patients with acute lymphocytic leukemia (ALL) who are in first or second complete response and have MRD greater than 0.1 percent.16,17 In addition, the FDA approved daratumumab in combination with bortezomib, melphalan, and prednisone for frontline treatment of MM, and the approval was based on a clinical trial that assessed MRD at multiple time points. The researchers found that MRD negativity was associated with improved progression-free survival (PFS), regardless of the treatment arm.17
Several large, ongoing phase III clinical trials are assessing therapies using MRD as an endpoint, but the reproducibility and standardization of an MRD assay remains a challenge. Deeper sensitivity – the ability of an MRD assay to detect a cancer cell against a background of healthy cells in a sample – allows for better outcomes predictions, while specificity – the accuracy and reliability to differentiate between
healthy and malignant cells – enables accurate quantitation of MRD.18,19 An assay that is validated and standardized in alignment with defined regulatory standards can help clinicians make treatment-related decisions. There are two regulatory pathways for clinical assays: (1) FDA clearance or approval, which is provided to the assay; or (2) Clinical Laboratory Improvement Amendments (CLIA) certification, which is provided to the laboratory performing the testing. FDA approval or clearance still requires that the laboratory performing the assay be CLIA-certified.
MRD in MM
Approximately 80 percent of adults with MM achieve CR, but 72 percent of those patients will experience disease progression, and survival rates after transplantation remain poor (the 10- to 15-year post-transplant survival rate is just 15%).20,21
In the Literature
Many studies have assessed MRD status related to disease progression and survival endpoints. MRD status is more predictive of overall survival (OS) than CR in both transplant- eligible and -ineligible patients, and a study published in 2014 in Blood found that approximately 58 percent of patients with MM in complete response were MRD-positive.22
A 2017 phase III study published in the New England Journal of Medicine compared the combination of daratumumab, lenalidomide, and dexamethasone versus lenalidomide and dexamethasone alone (control) in 569 patients with MM. They evaluated MRD status via NGS of bone marrow (BM) obtained from patients who had a suspected complete response. The rate of results below the MRD threshold was significantly higher in the daratumumab group than in the control group by three to five times at all evaluated thresholds (10-4, 10-5, and 10-6).23
A 2018 study published in the New England Journal of Medicine assessed 706 patients with newly diagnosed MM who were ineligible for transplantation to receive bortezomib, melphalan, and prednisone either alone (control) or with daratumumab. In the daratumumab group, 22.3 percent were MRD-negative at a threshold 10-5, compared with 6.2 percent in the control group (p<0.001). At all evaluated thresholds, patients who were MRD-negative had longer PFS than those who were MRD-positive.17
A meta-analysis published in 2016 in JAMA Oncology assessed 14 studies comprising 1,273 patients with MM and found that MRD negativity was associated with a median PFS of 54 months, compared with 26 months among MRD-positive patients.2
In the Guidelines
The NCCN Clinical Practice Guidelines In Oncology (NCCN Guidelines®), International Myeloma Working Group (IMWG) Consensus Criteria for Multiple Myeloma, and European Society for Medical Oncology (ESMO) Myeloma Clinical Practice Guide- lines recommend MRD assessment using a validated assay with a minimum sensitivity of 10-5.24,25 The IMWG response criteria recommend MRD testing after each treatment stage.25 The ESMO guidelines note, “There is a statistical relationship be- tween the achievement of complete response, MRD negativity, and PFS or OS.”26
 Luciano J. Costa, MD, PhD, of the Division of Hematology/Oncology at the University of Alabama, Birmingham, provides insights on the use of MRD in MM.
Luciano J. Costa, MD, PhD, of the Division of Hematology/Oncology at the University of Alabama, Birmingham, provides insights on the use of MRD in MM.
Can you discuss the use of MRD testing in patients with MM? In your opinion, how can MRD testing be used in clinical management?
There has long been a big gap in the management of patients with MM. Historically, we have relied on very old technologies – morphology of the BM and levels of paraproteins in serum and urine – to assess response to therapy, but these are suboptimal. While some of the heterogeneity of responses is intrinsic to the diverse biology of MM, it also reflects the imprecision of the traditional methods to assess disease response.
MRD helps shed bright light on the patients who have reached CR and who might have very different levels of remission. I see MRD as an evolution of the evaluation of MM disease burden. As MM therapies have evolved and a higher proportion of patients reach CR, it becomes more important to use better tools and new landmarks that can be correlated to outcomes. MRD testing can separate out groups of patients who have all reached CR but have very distinct prognosis.
With MRD, there are still more questions than answers, because the technology is relatively recent in MM, and the disease has a long natural history. It takes several years until a short-term endpoint such as MRD clearance can be correlated with long-term clinically meaningful endpoints such as PFS and OS. That being said, if we are willing to accept traditional response assessment as a short-term endpoint, we should also accept MRD.
What role does MRD play throughout the course of MM treatment? How does it impact treatment decisions, such as prior to therapeutic choice or transplantation?
That’s an excellent question and one for which we still don’t have definitive answers yet. MM treatment has been a stagnant package of therapy with few adjustments based on the depth of response. MRD assessment is the most valid technology to determine deep remissions. That’s a very important question for the near future, and we would like to see strategies that de-escalate therapy for patients who have persistent MRD-negative disease after intense initial therapy and escalate therapy for patients who have persistence of MRD and are, therefore, at high risk for recurrence.
What is the importance of an MRD assay’s sensitivity and specificity?
We have learned from several studies that, not surprisingly, sensitivity matters. When we look at the sensitivity of 10-4, which is usually reached by first-generation flow cytometry, the results are not very good: Most patients who are MRD-negative at this level will likely relapse within three to four years after treatment discontinuation. Outcomes predictions are increasingly better when we use the level of detection of 10-5 or 10-6.
As we move forward, it is important to have some laboratory standardization for sensitivity. The current IMWG white paper on MRD for MM calls for 10-5 as the definition of MRD negativity. Most of the data available at that level or deeper is based on NGS.
Describe the level of validation and/or standardization an assay would need to have in order for you to feel confident in its clinical actionability.
I believe one of the greatest assets of flow cytometry is also one of its great limitations: Flow cytometry can be done locally for most laboratories and academic institutions, so there is a quick turnaround, whereas NGS typically takes approximately seven days to produce results. However, with many laboratories conducting the test, there’s little assurance that the results will be the same, which can make it very difficult to interpret data legitimately and demonstrate a 10-5 result. So, validation is crucial. What I would consider the gold standard is a test that provides similar results when performed multiple times on samples from different institutions and has been anchored on data that correlates its output with clinically meaningful endpoints.
I think the existence of one major company providing NGS services creates that reassurance that it’s one platform – one test – and the same performance exhibited by NGS in clinical trials can be expected for a clinical sample that goes into analysis.
Should NGS-based MRD results be incorporated as a surrogate endpoint for clinical trials?
Absolutely; I think current and future clinical trials for MM should include MRD as an endpoint. I think that in a few years, it’s going to be very difficult to interpret any short-term results of an MM clinical trial without MRD data, particularly in the upfront setting where most modern regimens lead to high rates of remission.
MRD is definitely a surrogate endpoint, just like traditional response assessment. But I would ask and advocate that we use MRD as a primary endpoint in clinical trials, particularly those with a short-term endpoint in patients with newly diagnosed or early relapse MM.
Multicolor flow cytometry and NGS both have pros and cons; however, I do believe NGS is a more suited strategy for performance in clinical trials. NGS has very good validation, with a sensitivity level of up to 10-6. Sensitivity is an important aspect, and currently, the data and literature favor NGS-based MRD assessments as having the highest sensitivity.
Why did you choose to use NGS MRD as a method of assessment for your trial?
I have the privilege of leading “Monoclonal Antibody Sequence Therapy for Deep Remission in Multiple Myeloma (MASTER)” clinical trial that proposed a combination of lenalidomide, carfilzomib, daratumumab, and dexamethasone for upfront treatment followed by response- adapted consolidation therapy based on MRD assessment with one of the objectives being to determine whether it is feasible and safe to discontinue therapy in patients with sustained deep remissions. We use NGS because it has the highest level of sensitivity and a platform that tests at a central laboratory, so we don’t have to worry about changing the technical parameters of the test as we scale up to a larger group of patients at different sites. Just as important, if we are successful, the broad availability and reproducibility of the NGS test will assure physicians treating patients off-trial in the future that a negative MRD result in their patients will mean the same that it did for on-trial patients managed with this strategy.
MRD in ALL
While 85 to 90 percent of adult patients with ALL can achieve CR, 60 to 70 percent will experience disease recurrence, and survival in this adult population is poor. In addition, 30 to 50 percent of adult patients with ALL who have experienced CR are MRD-positive, which is associated with poorer survival.27,28
In the Literature
A meta-analysis published in 2017 in JAMA Oncology assessed 16 studies that included 2,076 adults with ALL to determine the relationship between MRD status and survival. MRD-negative status was associated with a 10-year event-free survival (EFS) rate of 64 percent, compared with 21 percent among those with MRD-positive disease.29
In the Guidelines
The NCCN Guidelines call MRD “an essential component of response evaluation” and recommends MRD testing for adult patients with ALL after initial induction and at other time points guided by the regimen used. The guideline also recommends MRD testing to identify patients in CR who are MRD-positive to identify those who are appropriate for treatment with blinatumomab. Specifically, the guideline recommends MRD testing with methods that reach a sensitivity of <10-4 and highlight that “MRD status appears to be a reliable predictor of clinical outcome following therapy.” The NCCN Guidelines also state that at diagnosis, there should be a “baseline characterization of leukemic clone to facilitate subsequent MRD analysis.”5 The American Society of Hematology (ASH) and College of American Pathology strongly recommend comprehensive molecular characterization at diagnosis to allow for subsequent MRD testing.30
 Aaron C. Logan, MD, PhD, of the Division of Hematology/Oncology at the University of California San Francisco, provides insights on the use of MRD in ALL.
Aaron C. Logan, MD, PhD, of the Division of Hematology/Oncology at the University of California San Francisco, provides insights on the use of MRD in ALL.
Can you discuss the use of MRD testing in patients with ALL? In your opinion, how can MRD testing be used in clinical management?
Various studies indicate that the presence of MRD after the initiation of multiagent chemotherapy in patients with ALL signifies high risk of disease relapse. It is now a fairly standard- accepted practice to measure MRD when assessing for CR after induction and throughout the course of therapy.
We’ve learned the importance of thorough MRD assessments from various studies, both in children and adults, and it’s clear that the presence of MRD at any time after the initiation of therapy signifies a risk of relapse. Measuring MRD offers an opportunity for the healthcare provider to intervene on that residual leukemia and change treatment to something that might work in a different way and be more effective in achieving an MRD-negative state and then potentially move onto allogeneic transplant.
For a long time, MRD testing has been somewhat difficult to access, particularly for adult patients with ALL. It has become easier because there are now commercially available tests (both flow cytometry and NGS). I think it should be standard practice to assess MRD at various timepoints, including at the end of induction and through consolidation and subsequent therapy to help guide treatment selection.
What role does MRD play throughout the course of ALL treatment? How does it impact treatment decisions, such as therapeutic choice or transplantation?
Tracking MRD levels helps assess the efficacy of the patient’s treatment regimen and make clinical decisions about the role for targeted therapy and subsequent allogeneic transplant.
In pediatric trials, MRD has been used in some protocols to identify patients who might benefit from either intensification or deintensification of therapy, but this is not part of the scope of adult ALL management. I think a critically important role for MRD testing in adult patients is to assess their response to multiagent chemotherapy early in the course of treatment. If patients are MRD-positive, they are at exceptionally high risk for relapse and poor survival. These are patients who would benefit from an alternative approach to treating their residual disease and should receive allogeneic transplant.
Some patients achieve MRD-negative remission, but subsequently become MRD-positive, and they are highly likely to relapse if continued on the same treatment protocol, thus there is value to serial measurement of MRD.
MRD persistence or relapse is now an opportunity to treat a patient with blinatumomab based on recent FDA approval of an expanded label, with a high (roughly 80%) likelihood of converting them to MRD negativity. I also think patients who have MRD relapse should receive allogeneic transplant, preferably after receiving additional treatment to achieve MRD negativity, at least until other approaches are shown to be as or more effective. Several studies demonstrate the importance of MRD negativity prior to transplant, because the likelihood of a successful transplant is much higher in these patients.
In the post-transplant setting, subsequent MRD is associated with near uniform mortality, so it’s important to follow MRD and potentially intervene on any measurable disease with blinatumomab or another treatment to prevent a post-transplant relapse.
Can you discuss how MRD negativity is associated with improved survival?
A study published in 2017 in JAMA Oncology showed by meta-analysis of several studies that MRD negativity does not guarantee continued remission, which is why serial MRD assessments should be performed. But patients who are MRD-negative early in the course of therapy are substantially more likely to remain in remission and have good survival, compared with those who are MRD-positive. The study also demonstrated that the hazard ratio for both OS and relapse-free survival for those who are MRD-positive was 0.28 for both adults and pediatric patients, representing a very significant impairment in these endpoints for patients with residual disease early in treatment.29
What is the importance of an assay’s sensitivity and specificity?
There are various tests for the assessment of quantification of residual disease. Flow cytometry is a test that many facilities use; however, there may be a difference in the level of sensitivity of a standard clinical diagnostic flow cytometry assay. Healthcare providers who plan to use flow cytometry should know the level of sensitivity. If their institution or preferred vendor is not providing a suitable level of MRD quantification, then providers should consider sending samples to a laboratory that does.
An alternative to flow cytometry is NGS, which has a higher level of sensitivity and is now commercially available to any U.S. provider. I think it is a very good alternative to flow cytometry, because it has a deeper level of sensitivity, potentially to 10-6, and that can lead to detection of lower levels of disease and potentially identify more patients who should be monitored more closely and intervened upon. The NGS assay may also detect MRD in the peripheral blood (PB), which is not feasible using flow cytometry because it’s not sensitive enough to detect the lower levels of disease that are typically found in PB, compared with those found in the BM.
Can you discuss MRD testing in BM versus PB?
A few studies have assessed how NGS based quantification of MRD compares in samples from the BM and PB. We conducted a study of samples from patients with ALL and found that there’s approximately 10 to 100 times as much ALL burden in the BM, compared with the PB in patients who are in remission.
I don’t think MRD assessment of the PB can absolutely replace BM, but NGS has a higher level of sensitivity that allows the opportunity to assess for MRD in the PB, and when disease is detected in the PB, it almost certainly is present at a higher level in the BM, which should lead the healthcare provider to alter the course of treatment. Another aspect that I think is intriguing and deserves more study is the rare instance of patients who have extramedullary disease. I have had some patients who have detectible disease burden in the PB using NGS; however, their BM is completely clean, and the MRD detected in the blood was actually associated with an extramedullary site of disease.
Introduction to the clonoSEQ Assay
The clonoSEQ® Assay* is an in vitro diagnostic test that uses PCR and NGS technology to detect and quantify MRD in lymphoid malignancies like ALL and MM. clonoSEQ is a highly accurate and sensitive assay that offers a standardized way to assess a patient’s disease burden over time in response to therapy or even in remission.31,32 The assay quantifies residual disease, tracks the identified sequences over time, and monitors for the emergence of new sequences.
The deep sensitivity of the clonoSEQ Assay has been shown to add insight to the evaluation of disease response to therapy, help predict patient outcomes, and detect early signs of relapse, enabling more timely decisions about how and when to intervene.1 Given sufficient sample input, clonoSEQ can detect measurable MRD at the level of a single cancer cell among 1 million healthy cells.33*
The clonoSEQ Assay recently received FDA clearance and De Novo designation for the detection and monitoring of MRD in bone marrow samples from patients with multiple myeloma or B-cell ALL. clonoSEQ is also available for use in other lymphoid cancers as a CLIA-regulated laboratory developed test service. clonoSEQ testing services are provided by Adaptive Biotechnologies.
In the Literature
The assay has generated peer-reviewed clinical evidence in MM and ALL. A 2018 study published in Blood found there was a high rate of discordance of MRD outcomes between NGS and flow cytometry testing at an MRD threshold of 10-4: Fifty-five pediatric patients with ALL were MRD-negative based on flow cytometry but were MRD-positive based on the clonoSEQ Assay, whereas 17 were MRD-positive by flow cytometry and MRD-negative by clonoSEQ. Those who were miscategorized by flow cytometry had worse EFS than those who were MRD-negative by both clonoSEQ and flow cytometry.9 Another study published in Blood in 2014 found that MRD-positive assessment by clonoSEQ was significantly associated with shorter time to progression and OS.22
A 2014 study published in Clinical Cancer Research showed that NGS can identify immunoglobulin heavy-chain genes in patients with B-cell ALL. MRD was detected by clonoSEQ in all flow cytometry-positive cases, and there were no falsenegative results for which MRD was only detected by flow cytometry but not NGS.34 Another 2014 study published in Biology of Blood and Marrow Transplantation showed that the use of clonoSEQ quantification in adults with ALL provides a standardized approach with sufficient sensitivity to quantify leukemia MRD in PB. The study used an older version of the clonoSEQ Assay (which has been continually optimized over time) to quantify MRD in 237 samples from 29 adults with B-cell ALL before and after allogeneic hematopoietic cell transplantation. Per post-HCT blood** samples, MRD ≥10-6 had 100 percent positive predictive value for relapse, with a median lead time of 89 days.35 Similarly, a study published in Blood in 2018 found that patients with the deepest levels of MRD (<10-6) as measured by clonoSEQ had longer progression-free survival (PFS) than patients with MRD levels from 10-6 to 10-5, 10-5 to 10-4, and >10-4 both prior to maintenance (P<0.001) and post-maintenance (P<0.001).36
Dr. Costa obtained his medical degree and subsequent PhD from Universidade de Sao Paulo in Brazil. He trained in hema- tology and medical oncology at the University of Colorado and in blood and marrow transplantation at the Mayo Clinic in Rochester, Minnesota. Dr. Costa is currently associate professor of medicine and senior clinical investigator at the University of Alabama at Birmingham Comprehensive Cancer Center where he also directs the Immune Effector Cellular Therapy Program. His primary interests are in the development of new therapies for MM, including new cellular therapies and immunotherapy.
Dr. Costa received compensation for his contribution.Dr. Logan is an associate professor in the Division of Hematology and Oncology at the University of California, San Francisco. Dr. Logan specializes in the management of acute leukemias and myelodysplastic syndromes using transplant and non- transplant modalities, including gene-modified cellular therapies. His research interests include ultrasensitive quantification of measurable residual disease and preemption of relapse, immune reconstitution following transplantation, and novel methods for preventing and treating graft-versus-host disease. Dr. Logan was offered but declined compensation for his contribution.
*clonoSEQ is available as an FDA-cleared in vitro diagnostic (IVD) test service provided by Adaptive Biotechnologies for use in B-cell acute lymphoblastic leukemia and multiple myeloma patients to detect and monitor measurable residual disease (MRD) in bone marrow samples. clonoSEQ is also available for use in other lymphoid cancers as a CLIA-regulated laboratory developed test (LDT) service provided by Adaptive Biotechnologies. clonoSEQ is available by prescription only. clonoSEQ results should always be used in combination with clinical examination, patient medical history, and other findings. Results may vary. False positive or false negative results may occur for reasons including, but not limited to: contamination, technical, and/or biological factors. For important information about the FDA-cleared uses of clonoSEQ, including test limitations, visit clonoSEQ.com/technical-summary.
**Blood-based MRD testing for patients with acute lymphoblastic leukemia is available as a CLIA-regulated laboratory developed test (LDT) service provided by Adaptive Biotechnologies. This use of clonoSEQ has not been approved or cleared by the FDA.
References
- Pulsipher MA, Carlson C, Langholz B, et al. IgH-V(D)J NGS-MRD measurement pre- and early post-allotransplant defines very low- and very high-risk ALL patients. Blood. 2015;125:3501-8.
- Munshi NC, Avet-Loiseau H, Rawstron AC, et al. Association of minimal residual disease with superior survival outcomes in patients with multiple myeloma: a meta-analysis. JAMA Oncol. 2016;3:28-35.
- ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). 2018 May 24. Identifier NCT02659293, Trial of carfilzomib, lenalidomide, dexamethasone versus lenalidomide alone after stem-cell transplant for multiple myeloma. Accessed on July 23, 2018, at https://clinicaltrials.gov/ct2/show/ NCT02659293.
- Taylor CR. From microscopy to whole slide digital images: a century and a half of image analysis. Appl Immunohistochem Mol Morphol. 2011;19:491-3.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Acute Lymphoblastic Leukemia V.1.2018. © National Comprehensive Cancer Network, Inc. 2018. All rights reserved. Accessed September 20, 2018. To view the most recent and complete version of the guideline, go online to NCCN.org.
- van Dongen JJ, van der Velden VH, Brüggemann M, et al. Minimal residual disease diagnostics in acute lymphoblastic leukemia: need for sensitive, fast, and standardized technologies. Blood. 2015;125:3996-4009.
- Campana D. Minimal residual disease in acute lymphoblastic leukemia. Semin Hematol. 2009;46:100-6.
- Han Y, Gu Y, Zhang AC, et al. Review: imaging technologies for flow cytometry. Lab Chip. 2016;16:4639-47.
- Wood B, Wu D, Crossley B, et al. Measurable residual disease detection by high-throughput sequencing improves risk stratification for pediatric B-ALL. Blood. 2018;131:1350-9.
- Anderson KC, Auclair D, Kelloff GJ, et al. The role of minimal residual disease testing in myeloma treatment selection and drug development: current value and future applications. Clin Cancer Res. 2017;23:3980-993.
- Kawasaki ES, Clark SS, Coyne MY, et al. Diagnosis of chronic myeloid and acute lymphocytic leukemias by detection of leukemia-specific mRNA sequences amplified in vitro. Proc Natl Acad Sci USA. 1988;85:5698-702.
- Paiva B, van Dongen JJ, Orfao A. New criteria for response assessment: role of minimal residual disease in multiple myeloma. Blood. 2015;125:3059-68.
- Carlson CS, Emerson RO, Sherwood AM, et al. Using synthetic templates to design an unbiased multiplex PCR assay. Nat Commun. 2013;4:2680.
- Reuter JA, Spacek DV, Snyder MP. High-throughput sequencing technologies. Mol Cell. 2015;58:586-97.
- Davies FE. Is molecular remission the goal of multiple myeloma therapy? Hematology Am Soc Hematol Educ Program. 2017;2017:205-11.
- Janssen Announces DARZALEX® (daratumumab) U.S. FDA Approval for Newly Diagnosed Patients with Multiple Myeloma who are Transplant Ineligible. Accessed on July 23, 2018, at www.jnj.com/media-center/press-releases/ janssen-announces-darzalex-daratumumab-us-fda-approval-for-newly- diagnosed-patients-with-multiple-myeloma-who-are-transplant-ineligible.
- Mateos MV, Dimopoulos MA, Cavo M, et al. Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med. 2018;378:518-28.
- Keeney M, Halley JG, Rhoads DD, et al. Marked variability in reported minimal residual disease lower level of detection of 4 hematolymphoid neoplasms: a survey of participants in the College of American Pathologists flow cytometry proficiency testing program. Arch Pathol Lab Med. 2015;139:1276-80.
- Saah AJ, Hoover DR. “Sensitivity” and “specificity” reconsidered: the meaning of these terms in analytical and diagnostic settings. Ann Intern Med. 1997;126:91-4.
- Landgren O, Devlin S, Boulad M, et al. Role of MRD status in relation to clinical outcomes in newly diagnosed multiple myeloma patients: a meta-analysis. Bone Marrow Transplant. 2016;51:1565-8.
- Martinez-Lopez J, Blade J, Mateos MV, et al. Long-term prognostic significance of response in multiple myeloma after stem cell transplantation. Blood. 2011;118:529-34.
- Martinez-Lopez J, Lahuerta JJ, Pepin F, et al. Prognostic value of deep sequencing method for minimal residual disease detection in multiple myeloma. Blood. 2014;123:3073-9.
- Dimopoulos MA, Oriol A, Nahi H, et al. Daratumumab, lenalidomide, and dexa- methasone for multiple myeloma. N Engl J Med. 2016;375:1319-31.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Multiple Myeloma. V.3.2018. © National Comprehensive Cancer Network, Inc. 2018. All rights reserved. Accessed September 20, 2018. To view the most recent and complete version of the guideline, go online to NCCN.org.
- Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17:e328-46.
- Moreau P, San Miguel J, Sonneveld P, et al. Multiple myeloma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):iv52-61.
- Terwilliger T, Abdul-Hay M. Acute lymphoblastic leukemia: a comprehensive review and 2017 update. Blood Cancer J. 2017;7:e577.
- U.S. Food and Drug Administration. Oncologic Drugs Advisory Committee Meeting: blinatumomab. Silver Springs, MD. March 7, 2018.
- Berry DA, Zhou S, Higley H, et al. Association of minimal residual disease with clinical outcome in pediatric and adult acute lymphoblastic leukemia: a meta-analysis. JAMA Oncol. 2017;3:e170580.
- Arber DA, Borowitz MJ, Cessna M, et al. Initial diagnostic workup of acute leukemia: guideline from the College of American Pathologists and the American Society of Hematology. Arch Pathol Lab Med. 2017;141:1342-93.
- Sherrod AM, Hari P, Mosse CA, et al. Minimal residual disease testing after stem cell transplantation for multiple myeloma. Bone Marrow Transplant. 2015;51:2-12.
- Faham M, Zheng J, Moorhead M, et al. Deep-sequencing approach for minimal residual disease detection in acute lymphoblastic leukemia. Blood. 2012;120:5173-80.
- Sala Torra O, Othus M, Williamson DW, et al. Next-generation sequencing in adult B cell acute lymphoblastic leukemia patients. Biol Blood Marrow Transplant. 2017;23:691-6.
- Wu D, Emerson RO, Sherwood A, et al. Detection of minimal residual disease in B lymphoblastic leukemia by high-throughput sequencing of IGH. Clin Cancer Res. 2014;20:4540-8.
- Logan AC, Vashi N, Faham M, et al. Immunoglobulin and T-cell receptor gene high-throughput sequencing quantifies minimal residual disease in acute lymphoblastic leukemia and predicts post-transplant relapse and survival. Biol Blood Marrow Transplant. 2014;20:1307-13.
- Perrot A, Lauwers-Cances V, Corre J, et al. Minimal residual disease negativity using deep sequencing is a major prognostic factor in multiple myeloma. Blood. 2018. doi:10.1182/blood 2018-06-858613.
Adaptive Biotechnologies is the manufacturer of the clonoSEQ Assay and provided funding for this advertisement.
This is a paid sponsorship by Adaptive Biotechnologies. Academy for Healthcare Learning conducted all interviews and developed all content independently of Adaptive Biotechnologies.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.