
During the recent American College of Rheumatology (ACR) Convergence 2021 conference, there was an intriguing talk targeting adult rheumatologists on how to manage adult patients with juvenile idiopathic arthritis (JIA). Dr. Mara Becker, a professor of pediatrics at Duke University School of Medicine and a pediatric rheumatologist, spoke on the management of adults with JIA including uveitis and macrophage activation syndrome (MAS).
Dr. Becker opened by discussing current evidence and recommendations for monitoring and treatment of JIA-associated uveitis. There are two major phenotypes of anterior uveitis in JIA. First, chronic anterior uveitis is seen in oligoarticular JIA or RF- polyarticular subtypes, often ANA positive, seen in younger children with insidious onset, and often requires systemic therapy. The second type is acute anterior uveitis, seen in the enthesitis-related arthritis (ERA) or spondyloarthropathy subtype, often with associated HLA-B27 positivity; this presents with sudden-onset of unilateral, red painful eye and is easily treated with topical steroids and often does not often require systemic therapy.
“Up to 20% [of children with JIA-associated uveitis] may have vision loss,” Dr. Becker said. “Screening is essential to identify, treat and mitigate risks of long-term sequalae.”
Reviewing Recent Guidelines
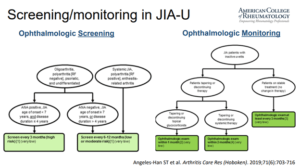
Next, the 2019 American College of Rheumatology/Arthritis Foundation Guidelines on Screening, Monitoring, and Treatment of JIA-associated uveitis was reviewed. High-risk features for JIA-associated uveitis require ophthalmology screening every 3 months; these features include ANA positivity, early age of JIA onset < 7 years of age, and disease duration less than or equal to 4 years (click Figure 1). Systemic immune-modulating therapy is recommended if activity cannot be controlled within 3 months, given long-term sequalae of topical steroids (such as glaucoma and cataracts) and the fact early DMARD therapy decreases the chance of requiring ophthalmologic surgeries, she explained. During the Q&A session, Dr. Becker recommended once JIA patients are adults over 18 years of age to continue screening by an ophthalmologist once a year.
Next, Dr. Becker discussed the clinical spectrum of JIA and how to recognize disease characteristics that may impact care in adulthood. The persistence of JIA symptoms in adulthood ranged from around 50% to 90% in some studies. She reviewed data that demonstrated early effective treatment is key to prevent long-term adverse outcomes. Finally, Dr. Becker discussed how it is important to recognize that adult patients with JIA may have increased cardiovascular risk related to comorbid cardiovascular risk factors, treatment-related complications (such as corticosteroids), increased inflammation and subclinical arterial damage.
The Complications of Juvenile Idiopathic Arthritis
Dr. Becker also discussed systemic JIA and its complications, noting that “while treatments targeting IL-1 and IL-6 cytokines implicated in the pathway of sJIA are now available, 20 to 40% of patients [with sJIA] still do not respond to treatment.”
Macrophage activation syndrome (MAS) is a complication seen in around 15% of patients with systemic JIA. Laboratory features that may be clues to diagnosis include hyperferritinemia, pancytopenia, elevated liver enzymes, elevated triglycerides, low fibrinogen, and paradoxically low sedimentation rate (ESR), Dr. Becker explained. She also discusses the new 2016 MAS Classification Criteria, now being used more frequently over the former 2004 HLH criteria. First line treatments for MAS flare include glucocorticoids, cyclosporine A, and Anakinra; resistant MAS may be treated with the HLH-2004 treatment protocol including etoposide. Some trials are exploring emerging therapies in MAS including JAK inhibitors and emapalumab (monoclonal antibody against IFN-γ), as well as IL-18 binding protein (Tadekinig alfa) in one case report.
Finally, Dr. Becker discussed systemic JIA associated lung disease, an entity observed in the last 10 years characterized by mild tachypnea, chronic cough and digital clubbing with high risk of mortality. Pathology demonstrates pulmonary alveolar proteinosis (PAP), endogenous lipid pneumonia, and fibrosis. BAL fluid shows elevated levels of IL-18, CXCL9 and CXCL10. Tissue gene expression profiling shows signature suggestive of IFNy-induced pulmonary inflammation, Becker explains. Risk factors for this complication, including sJIA diagnosis less than 2 years of age, having recurrent MAS, having high IL-18 levels and adverse reactions to tocilizumab. Finally, she referenced a new study by Hollenbroch and Ombrello et al which demonstrated association of this lung disease as a drug hypersensitivity reaction with HLA-DRB1*15.
In her concluding remarks, Dr. Becker emphasized early treatment in JIA is important for improved long-term outcomes in adulthood. She noted that understanding the mechanisms of clinical heterogeneity of systemic JIA at a molecular and biologic level is novel, and also said that targeted therapies are emerging against IL-18 and IFN-y (important contributors to MAS and other serious sJIA comorbidities).
Source: 7S403. Management of Adults with JIA: Uveitis, MAS & More, ACR Convergence 2021







 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.