In patients with a first unprovoked venous thromboembolism (VTE), the long-term risks and consequences of anticoagulant-related major bleeding are considerable based on a recent systematic review and meta-analysis published in the Annals of Internal Medicine.1
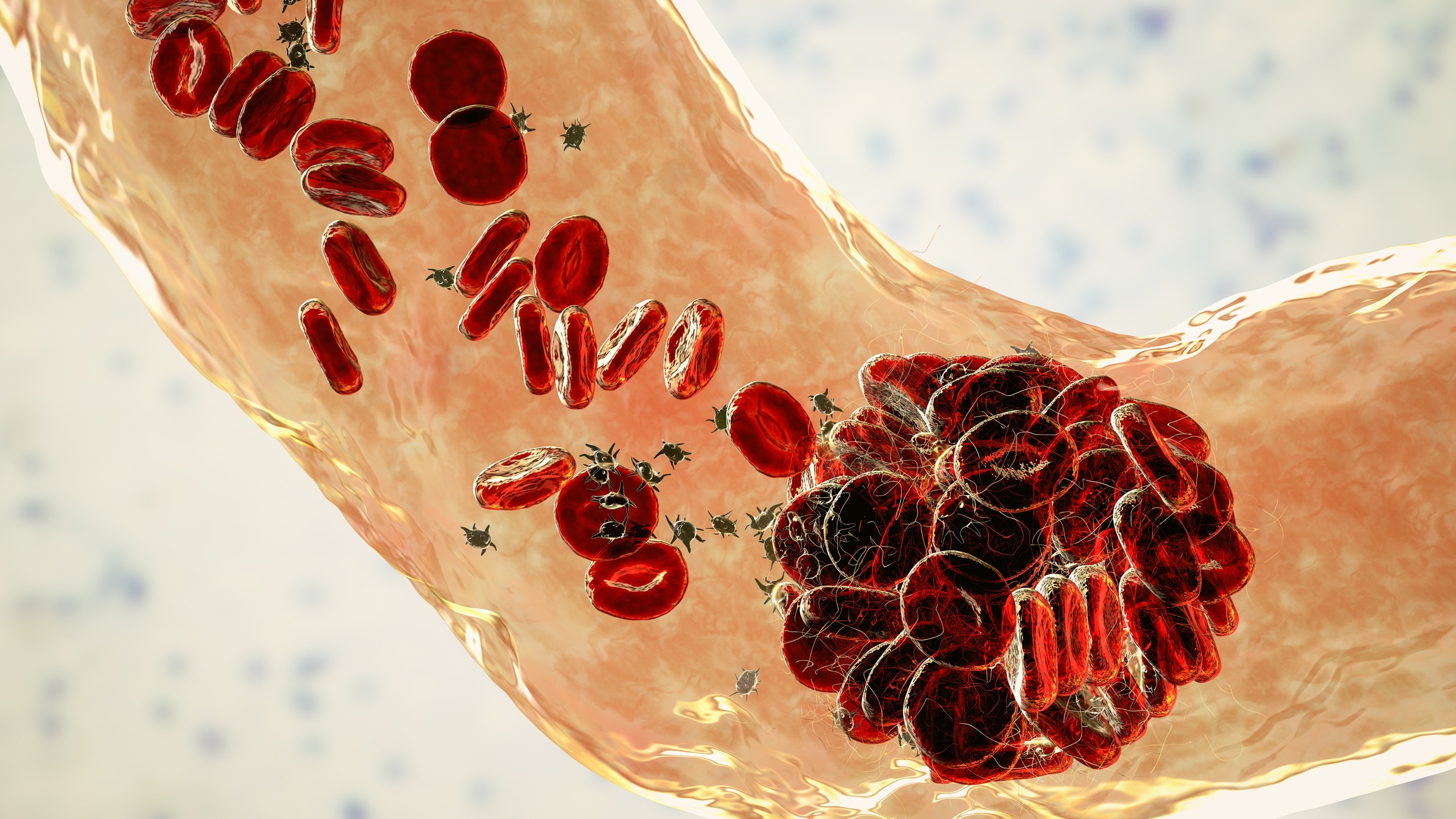
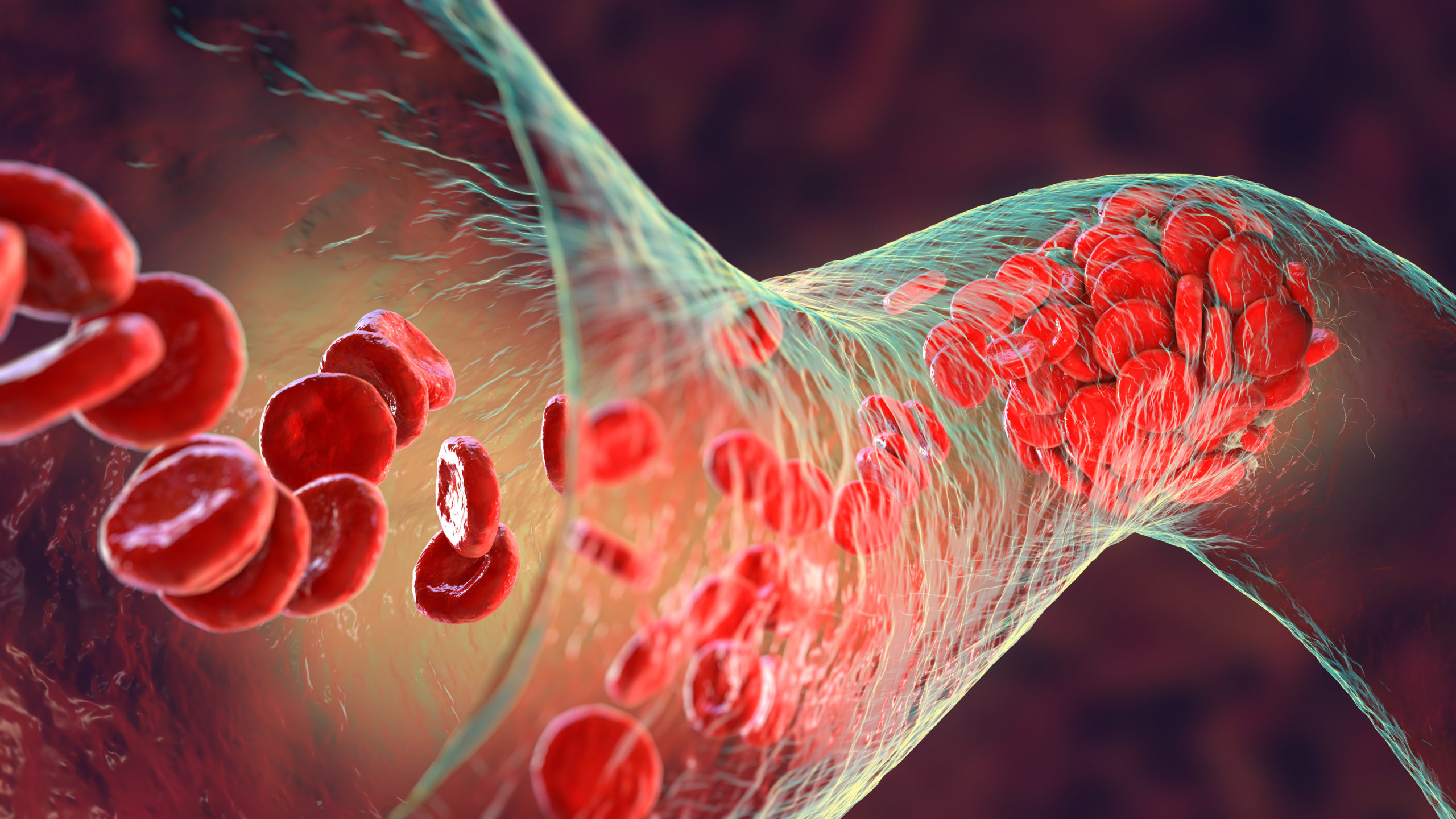
Deep venous thrombosis (DVT) is a blood clot that occurs in the deep veins of the body. They are categorized as “provoked” or “unprovoked.” Provoked DVTs occur in the presence of acute or chronic risk factors. Acute or transient risk factors include recent surgery, hospitalization, pregnancy or injury leading to prolonged hospitalization. Chronic or long-term risk factors include cancer, inflammatory or autoimmune disorders, chronic infections, and chronic immobility. Unprovoked DVTs occur in the absence of a clear risk factor. Recommended anticoagulants include vitamin K antagonists (VKA) or direct oral anticoagulants (DOACs) over aspirin. Per the American Society of Hematology (ASH) 2020 guidelines for the management of VTE, the recommended duration of anticoagulation for an unprovoked DVT is 3-6 months however should be continued indefinitely in those without a high risk of bleeding.2
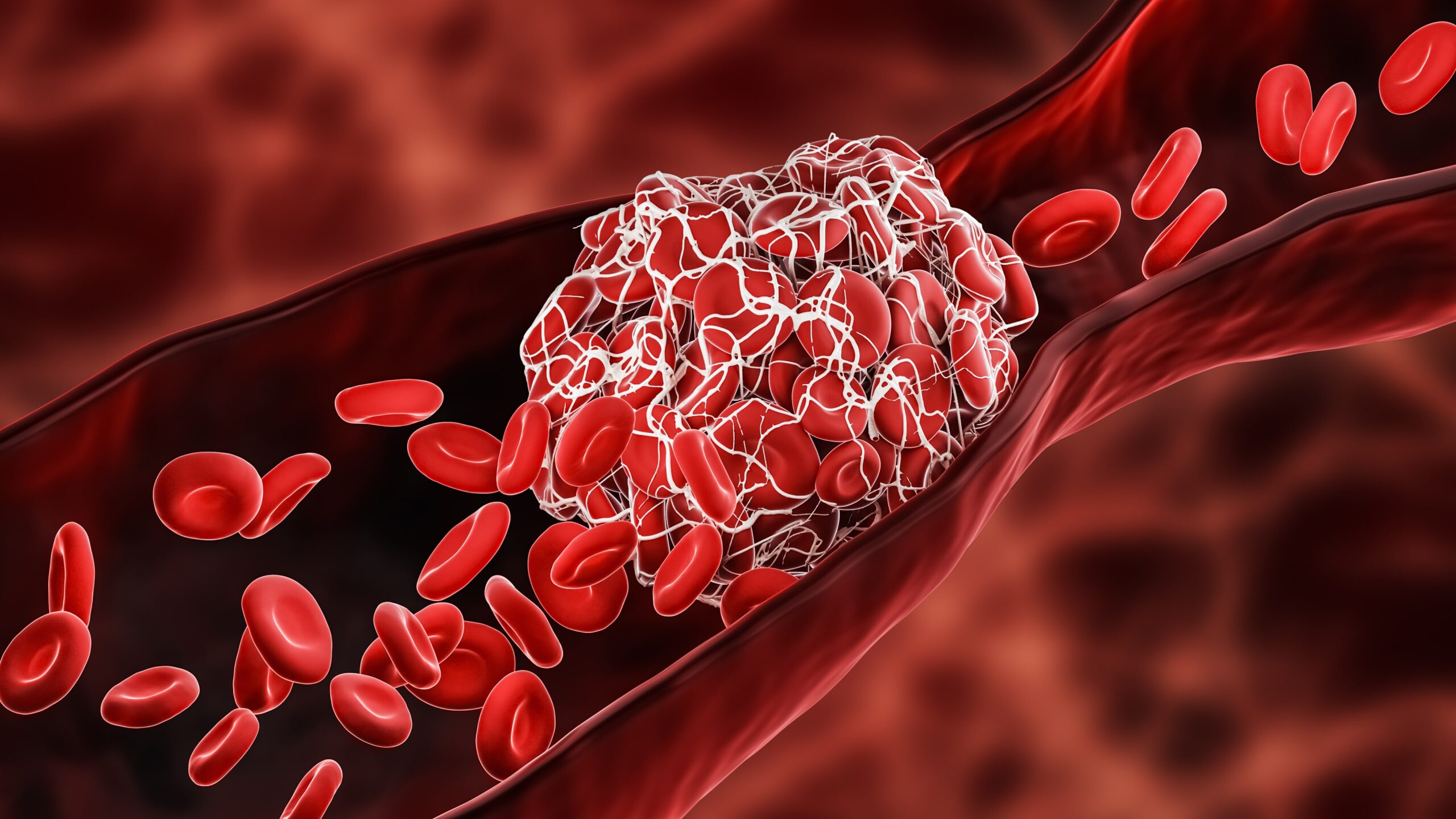
Recently, in a meta-analysis published in 2021, the risk of major bleeding in patients with unprovoked DVTs receiving anticoagulation beyond the initial 6 months was evaluated.2 In this study, a little under 10,000 patients received a VKA while approximately 7,200 patients received a DOAC. The incidence of major bleeding per 100 person-years was 1.74 vs. 1.12 events for VKAs and DOACs, respectively. The incidence of major bleeding with VKAs and DOACs was noted to be statistically significantly higher in those older than 65 years of age, creatinine clearance less than 50 mL/min, history of bleeding, concomitant use of antiplatelet therapy, or a hemoglobin less than 10. Surprisingly the case-fatality rate of major bleeding was 8.3% vs. 9.7% for VKAs and DOACs, respectively.1 While DOACs have been considered to be “safer,” they have been known to have higher bleeding events than VKAs3 but lower mortality rates compared to VKAs in the elderly.3 This is in contrast to the meta-analysis mentioned previously.
These studies raise several important questions for clinicians. First, how long is too long when treating patients with unprovoked DVTs? Second, how safe are DOACs compared to VKAs when treating unprovoked DVTs? Perhaps, we need to evaluate patients with unprovoked DVTs closely to better assess for all potential thrombotic and bleeding risk factors. Is the risk of clotting worth more or less than the risk of bleeding?
References
- Khan F, Tritschler T, Kimpton M, et al. Long-term risk for major bleeding during extended oral anticoagulant therapy for first unprovoked venous thromboembolism: a systematic review and meta-analysis. Ann Intern Med. Published online September 14, 2021:M21-1094.
- Ortel TL, Neumann I, Ageno W, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Advances. 2020;4(19):4693-4738.
- Poli D, Antonucci E, Bertù L, et al. Very elderly patients with venous thromboembolism on oral anticoagulation with VKAs or DOACs: Results from the prospective multicenter START2-Register Study. Thrombosis Research. 2019;183:28-32.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.