
Researchers conducted a trial to compare the incidence of permanent pacemaker (PP) implantation following either biatrial ablation (BA) or left atrial ablation (LAA) with simultaneous coronary bypass (CB) in patients with long–standing persistent atrial fibrillation (AF). They reported that BA with simultaneous myocardial revascularization was associated with a high risk of atrioventricular (AV) block, which required postoperative permanent PP implantation. The study was published in Kardiologiia.
However, in general, the total incidence of permanent PP implementation for cardiac conduction system dysfunction after CD and LAA or BA surgery “did not differ between the treatment groups both in early and late postoperative periods,” according to lead author, A. T. Kalybekova, PhD, and colleagues
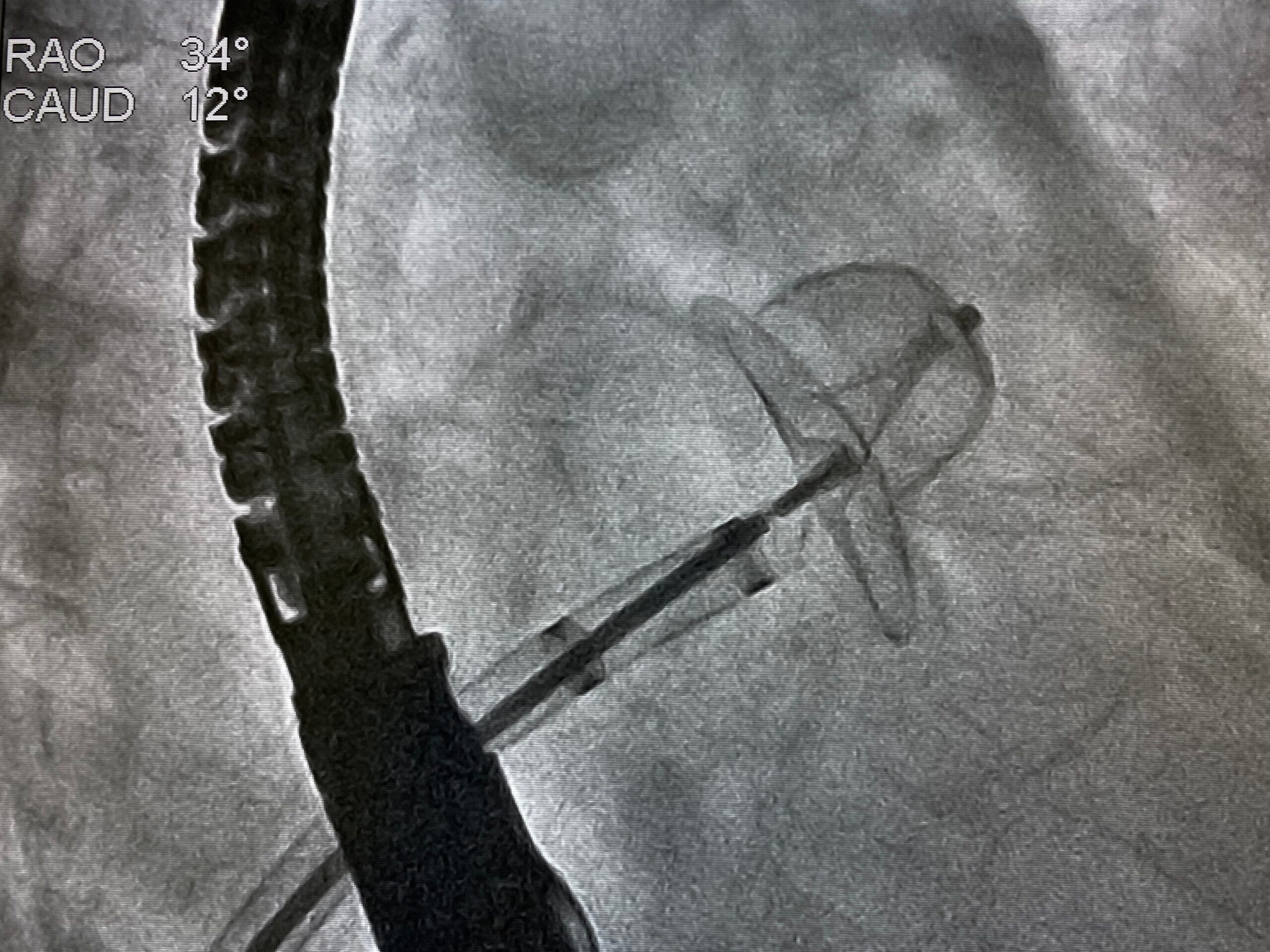
The trial enrolled a total of 116 patients with long–term persistent AF who were indicated for CB into two groups of 58 patients. Group 1 underwent BA combined with CB, whereas group 2 underwent isolated LAA with simultaneous CB in the setting of artificial circulation. PP implantation was assessed during the early (up to 30 days) and late (up to 60 months) postoperative periods.
Overall, nine total PPs were implanted, six in the BA group and three in the LAA group (odds ratio [OR], 0.5; 95 % confidence interval [CI], 0.1–2.4; P = 0.490). Most implantations occurred in the early postoperative period, with five patients in the BA group and two patients in the LAA group requiring PPs (OR, 0.4; 95% CI, 0.0–2.5; P = 0.438). One patient from the BA group and one patient from the LAA group were implanted in the late postoperative period at 30 and 54 months, respectively, due to the development of sick sinus syndrome.
The article reported that the causes for PP implantation in the BA group included complete AV block in 9% of cases (95 % CI, 4–19 %) and sinus node dysfunction and junctional rhythm in 2% of cases (95 % CI, 0–9). Comparatively, the LAA group had statistically significant reduced incidence of AV block (0 cases, P = 0.047). The most common reason for PP implantation in the LAA group was the development of sinus node dysfunction in 5% of patients (3 cases, 95 % CI, 2–14).
While the total incidence of permanent PP implementation required after operation did not differ significantly between patients undergoing BA or LAA with simultaneous CB, utilizing BA in the surgical procedure appeared to be accompanied by a higher risk of AV block, which requires PP implantation.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.