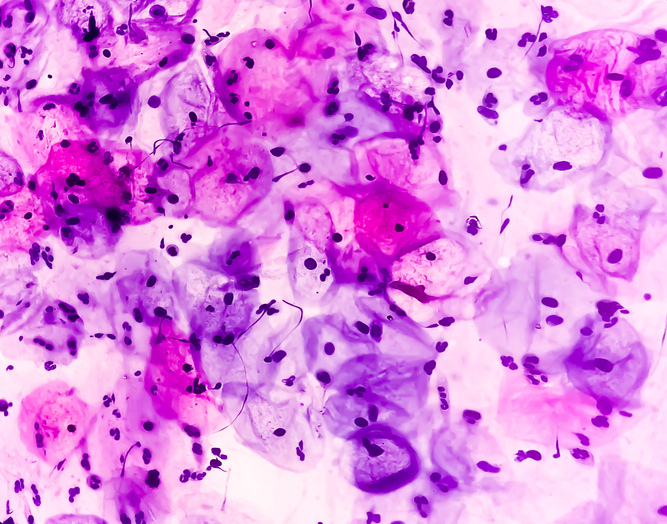
Several studies presented at the 2018 American Society of Hematology Annual Meeting showed long-term efficacy results of chimeric antigen receptor (CAR) T-cell therapies.
The ZUMA-1 trial assessed the CAR T-cell therapy axicabtagene ciloleucel in patients with relapsed/refractory diffuse large B-cell lymphoma (DLBCL). After a median follow-up of 27.1 months for 101 evaluable patients, 83% achieved an objective response, 58% had a complete response (CR), and 39% reported enduring responses. The median overall survival (OS) was not reached, and the median progression-free survival was 5.9 months. Nearly half of evaluable patients (48%; n=52) had grade ≥3 serious adverse events (AEs), including cytokine release syndrome (CRS; n=12; 11%) and neurologic events (n=35; 32%).
Five studies presented at #ASH18 highlighted the long-term effectiveness of CAR T-cell therapies in some patients and analyzed how combinations and transplantation after CAR T-cell therapy can affect response. See our poster for more info on CAR T cells https://t.co/Ow0TVO1era pic.twitter.com/Ayuvo6WZnN
— Nature Reviews Drug Discovery (@NatRevDrugDisc) December 3, 2018
The pivotal, phase II ELIANA trial assessed tisagenlecleucel in pediatric and young adult patients with relapsed/refractory acute lymphocytic leukemia. Among 79 evaluable patients, 82% achieved CR or CR with incomplete blood count recovery within 3 months of infusion, and among these patients, 98% were minimal residual disease-negative. The relapse-free survival rate was 62% at 24 months, and the median duration of remission and median OS were not reached. The probability of OS was 76% at 12 months and 66% at 24 months. There were no new safety signals: Grade 3/4 CRS occurred in 49% of patients. Within 8 weeks of infusion, 13% of patients experienced grade 3 neurologic events.
Last speaker on CAR T media briefing is Dr. Corinne Summers of @seattlechildren and @fredhutch speaking on long term follow up of CAR T-cell therapy in pediatric patients (abstract #967: https://t.co/HFFkG7R90B) #ASH18
— Molly McElroy (@mwmcelroy) December 1, 2018
The single-arm, open-label, multicenter, global, pivotal, phase II JULIET study assessed tisagenlecleucel in patients with relapsed/refractory DLBCL. After 19 months of follow-up of 99 evaluable patients, the overall response rate was 54%, including a 40% CR rate and 13% partial response (PR) rate. In addition, 54% of patients who initially had a PR achieved a CR. The median duration of remission was not reached. The relapse-free probability was 66% at 6 months and remained at 64% at 12 and 18 months. The median OS for all infused patients was 11.1 months and was not reached for patients in CR. The OS probability was 48% at 12 months and 43% at 18 months. AEs were consistent with previous reporting. Grade 3/4 CRS occurred 23% of patients, while grade 3/4 neurologic events were observed in 11% of patients.
CAR T-cell therapy is cost-effective for pediatric ALL.
A study identifies a biomarker that signals better response to CAR T-cell therapy.
Source: ASH





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.