Anthracyclines, such as doxorubicin, are a class of chemotherapy drugs used for both solid and hematologic malignancies. Dr. Eric Yang, a specialist in cardio-oncology at UCLA, notes that:
“Despite [their] known cardiotoxic properties… strategies to effectively diagnose and prevent the onset of cardiac dysfunction and heart failure remain elusive. Randomized controlled trials of neurohormonal agents, which have their established roles in heart failure with reduced ejection fraction, have unfortunately yielded little and/or no efficacy against the development of left ventricular dysfunction. However, with the impressive data of flozins as a new weapon in the arena of heart failure, it is an attractive drug class to study in the role of cardioprotection and treatment of cardiotoxicity.
Indeed, prior in vitro human cells and rat models studies, SGLT2 inhibitors appear to protect against anthracycline induced left ventricular (LV) dysfunction by reducing cardiomyocyte apoptosis and inflammatory cytokine expression.”
A recently published retrospective case-control study suggests that SGLT2 inhibitors (SGLT2i) may hold promise in the clinical world.
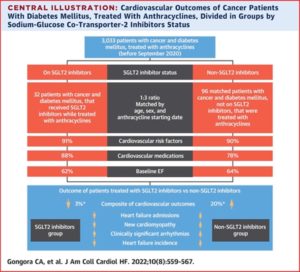
Researchers reviewed electronic medical records of the Massachusetts General Brigham system for diabetic patients undergoing anthracycline treatment. They compared SGLT2i users (n = 32) to non-users (n = 96) in a 1:3 ratio matched by age, sex, and anthracycline initiation date.
The results showed that SGLT2i use was associated with a significant benefit in terms of both efficacy and safety over a median follow-up period of 1.5 years. On the efficacy front, 20% of the non-SGLT2i patients had an adverse cardiovascular outcome (defined by new onset heart failure (HF), HF admission, or LV dysfunction) compared with only 3% of the SGLT2i patients (p = 0.025) .
Regarding safety, the SGLT2i cohort had reduced all-cause mortality: non-SGLT2i patients compared to SGLT2i patients had a hazard ratio of 4.7 ([95% CI: 1.5-15.1]; P = 0.005). Additionally, the rate of urinary tract infections (UTIs) and a composite of neutropenic fever and sepsis were lower in the SGLT2i group, albeit the overall incidence was low.
In response to these findings, Dr. Yang states that:
“As exciting and promising as this may be, it is important to realize this was overall a small study, with only 32 patients on SGLT2i with diabetes and cancer being followed. In addition, association is not causation, and like many agents that had cardioprotective promise, were not proven to be effective in prospective, randomized controlled trials. It is also important to note that non-diabetics were not studied in this analysis, as it is not standard of care outside of heart failure and diabetes to initiate these medications–do they need to be evaluated?
All these questions require a large scale, well conducted study, like CECCY, SUCCOUR, and other cardio-oncology trials that hopefully will help us identify–or exclude–what will help attenuate cardiac risk with anthracyclines.
However, an even bigger question, should these cardioprotective effects pan out, is the big why. What are the mechanistic links between the effects of SGLT2i in interfering with the proapoptotic mechanisms of anthracyclines–thought to be driven by oxidative stress, iron overload, and topoisomerase 2-beta targeting? This is a question that the scientific community needs to tackle, particularly as it may yield invaluable insights into ‘traditional’ forms of heart failure and cardiomyopathy, in order for us to advance the cardiovascular field.”
As Dr. Yang notes, this study provides a glimmer of hope that perhaps there is a brighter future ahead in the world of heart failure, but larger scale clinical and mechanistic trials are needed.
From @jaccjournals https://t.co/AOKHRmiSHV SGLT2 inhibitors in anthracycline treated patients. Great work by @TomasNeilan @dineshpmcc1 and colleagues #cardioonc. Would be a great clinical trial as suggested.
— Avirup Guha, MBBS, MPH, FICOS, FACC, FAHA (@avirupguha) June 8, 2022
References.
Gongora C, Drobni Z, Quinaglia Araujo Costa Silva T, et al. Sodium-Glucose Co-Transporter-2 Inhibitors and Cardiac Outcomes Among Patients Treated With Anthracyclines. J Am Coll Cardiol HF. 2022 Aug, 10 (8) 559–567.https://doi.org/10.1016/j.jchf.2022.03.006
Khouri M, Greene S, et al. Sodium-Glucose Co-Transporter-2 Inhibitor Therapy During Anthracycline Treatment. J Am Coll Cardiol HF. 2022 Aug, 10 (8) 568–570.https://doi.org/10.1016/j.jchf.2022.04.014
Octavia Y, Tocchetti CG, Gabrielson KL, Janssens S, Crijns HJ, Moens AL. Doxorubicin-induced cardiomyopathy: from molecular mechanisms to therapeutic strategies. J Mol Cell Cardiol. 2012;52(6):1213-1225. doi:10.1016/j.yjmcc.2012.03.006



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.