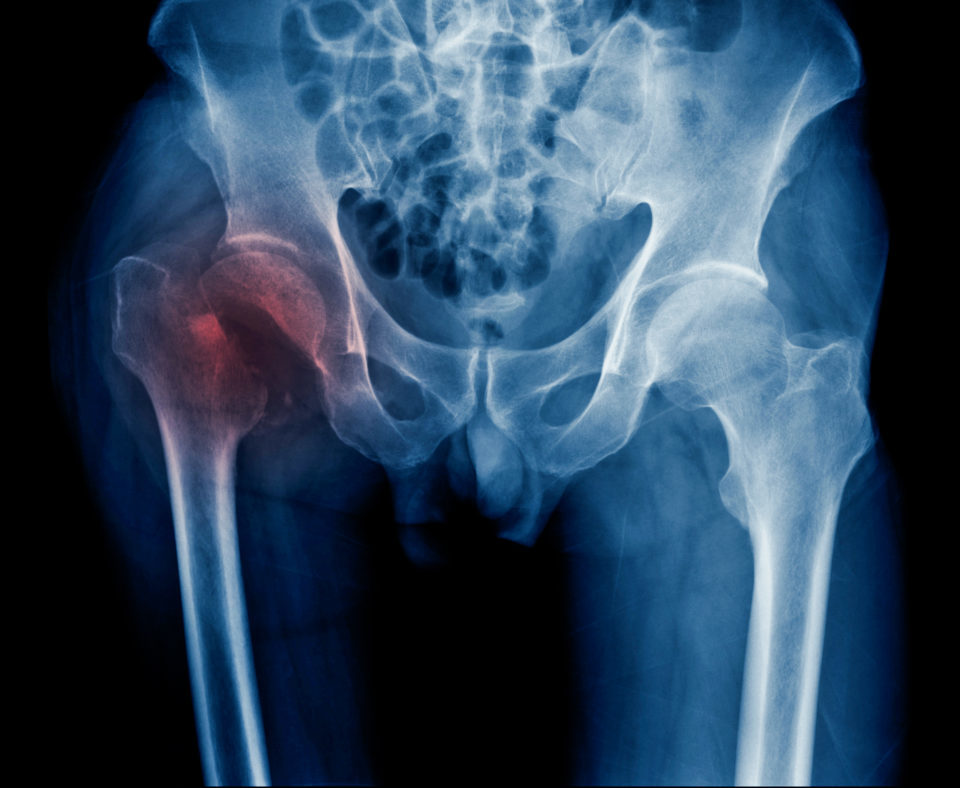
An estimated 300,000 hip fractures occur in the U.S. each year—a number that is expected to double with the aging population. About half of hip fractures are intertrochanteric fractures, but postoperative outcomes tend to be poor, including a high risk of mortality as well as poorer functional and quality of life outcomes. Certain risk factors for such poor outcomes are age and sex—which cannot be modified. One thing that can be modified, though, is preoperative planning. And according to a study published in JAMA Network Open, computer-assisted virtual planning in cases of intertrochanteric hip fracture may improve postoperative complications, including mortality risk.
Researchers retrospectively reviewed data from a level one trauma center database on 1,445 intertrochanteric hip fracture patients aged 65 years and older treated between Jan. 1, 2009, and March 31, 2018. Patients were stratified into two groups: those who received computer-assisted virtual preoperative planning (virtual planning group; n=558), and those who received conventional preoperative planning (conventional planning group; n=887). After excluding patients from both the virtual (n=93) and conventional (n=131) planning groups, the final analysis included 1,221 patients. The main outcomes were 90-day all-cause mortality and postoperative complications including myocardial infarction, heart failure, stroke, kidney failure, and sepsis; secondary outcomes included 90-day outpatient visits, hospital readmissions, and reoperations.
The mean (SD) age among the 1,221 patients in the final analysis was 73.2 (12.3) years; three-quarters of patients (n=927; 75.9%) were female. The virtual planning group had 465 patients, and the conventional planning group had 756 patients; 814 patients were propensity score-matched, with 407 patients in each group. In the matched analysis, the virtual planning group, compared to the conventional planning group, had a lower rate of mortality (9.1% vs. 13.5%; hazard ratio [HR]=0.64; 95% confidence interval [CI], 0.41 to 0.99; P=0.04) and postoperative complications (6.1% vs. 10.8%; HR=0.54; 95% CI, 0.32 to 0.90; P=0.02). Outpatient visits did not largely differ between the virtual and conventional planning groups (1.51 vs. 1.48 incidents per 30 person-days; incidence rate ratio [IRR]=0.90; 95% CI, 0.49 to 1.68; P=0.75); hospital readmission rates were also similar (0.99 vs. 1.01 incidents per 30 person-days, respectively; IRR=0.91; 95% CI, 0.49 to 1.67; P=0.76). The reoperation rate was lower in the virtual planning group than the conventional planning group (0.76 vs. 0.97 incidents per 30 person-days; IRR=0.41; 95% CI, 0.22 to 0.76; P=0.01).
“These findings support the use of preoperative planning based on computer-assisted virtual surgical technology for older patients with intertrochanteric fractures. Further studies are needed to define the role of virtual surgical technology,” the study authors concluded.







 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.