People who identify as LGBTQ, transgender, or gender non-conforming face significant challenges in accessing health care that fits their needs and makes them feel comfortable. A presentation at the annual conference of the Hematology/Oncology Pharmacy Association offered guidance for oncology clinicians to better care for this population.
“Cancer Screening and Care for Transgender and Gender Non-Conforming Patients,” presented by Maya Leiva, PharmD, BCOP, hematology and oncology advanced practice pharmacist at the Inova Schar Cancer Institute in Fairfax, VA, shared data that indicate that 3% of the U.S. population may identify as transgender or gender non-conforming. And the number of people who identify as LGBTQ is at its highest level ever documents—and likely growing: 5.6% of U.S. adults in a 2017 Gallup poll, representing a significant increase from a 2012 Gallup poll.
Patients in this demographic often face problems with insurance approvals for their healthcare needs, negative experiences with healthcare providers, fear of being mistreated, and ability to afford health insurance.
Dr. Leiva encouraged practitioners to apply trauma-informed care to this population. Trauma-informed care “avoids discrimination by embracing a person’s identity, reduces harm by validating and emphasizing a person’s feelings and value, and acknowledges gaps in data while still treating a patient ethically,” Dr. Leiva said.
In the world of cancer care, people who identify as transgender or gender non-conforming also face additional challenges related to screening. Clinicians should think carefully and engage in open discussions with patients about what types of screening they need. It’s important to educate transgender and gender non-conforming patients about why they may need screening for conditions that affect a gender they may on identify with, Dr. Leiva said. These conversations should be based on organ assessment, as opposed to traditional gender assignments.
Dr. Leiva also encouraged clinicians to focus on joint decision-making in order to provide the best care. This may involve flexibility regarding the environment where care is provided and the timing of examinations and procedures, particularly in those who are transitioning from one gender to another.
Additional insights included:
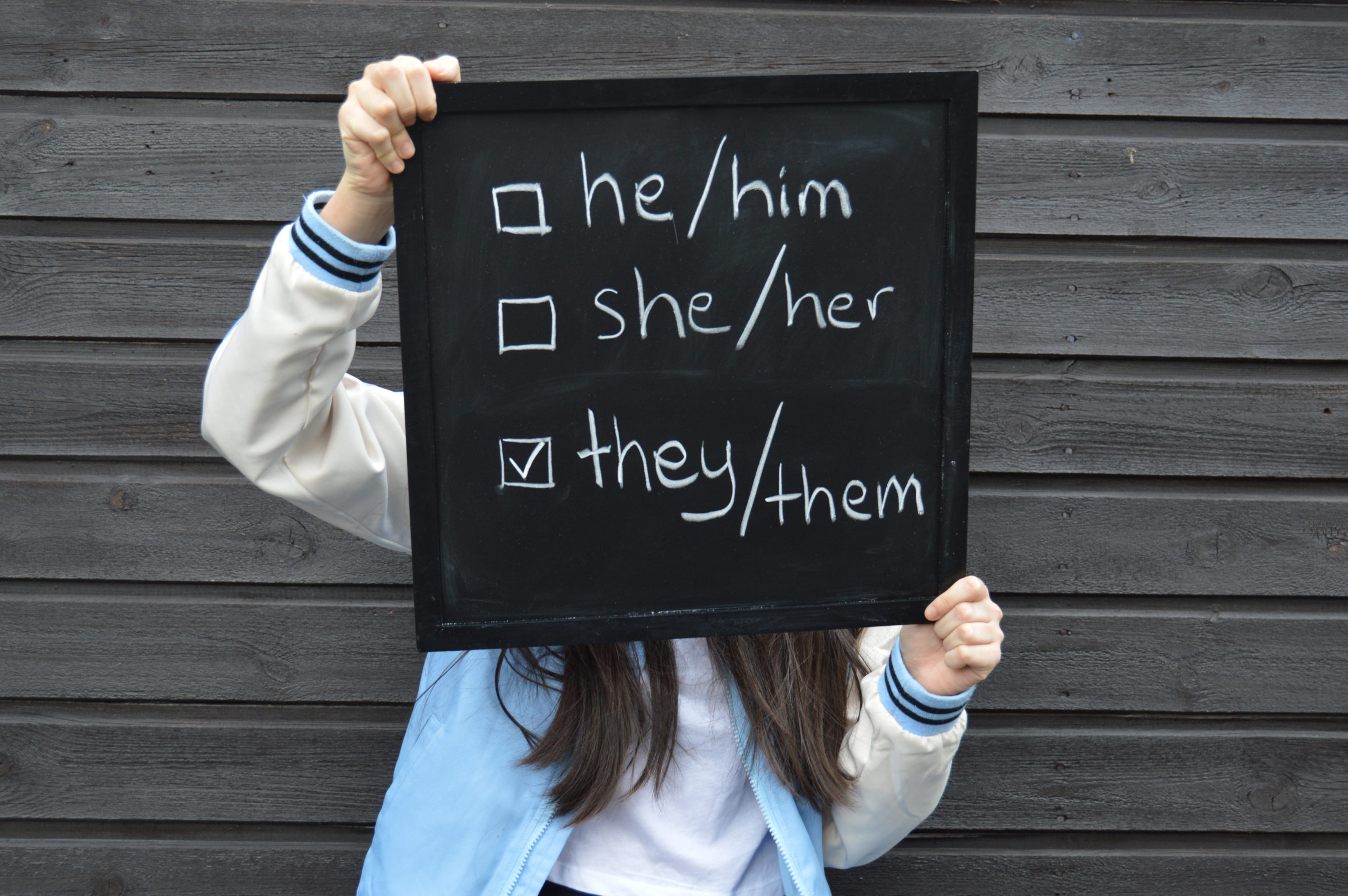
- Collect information on sexual orientation (SO), gender Identity (GI), preferred pronouns, and preferred name as early as possible in the process.
- Confirm SO, GI, preferred pronouns, and preferred name at each encounter, as it may be fluid.
- Use the least-gendered language possible or the terms the patient uses to describe body parts.
- Use warm hand-offs among other members of the multidisciplinary team (nursing, pharmacy, and other clinicians) so that they are aware of patient preferences. This will help prevent miscommunication and misgendering.
- Be aware of the increased risk of insurance rejections, which may cause treatment delays.
- When referring patients to support groups and other resources, keep in mind that those environments can be highly gendered. Help patients seek support that may be a better fit, possibly online.
- Use general language and terminology in all patient handouts and education.







 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.