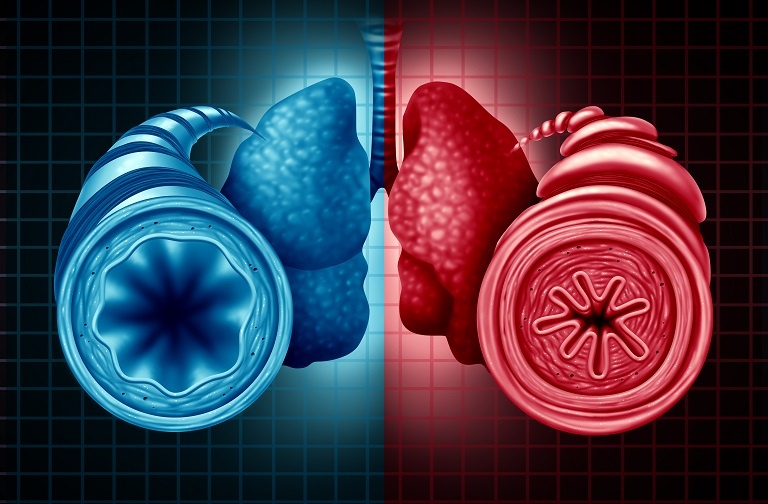
Tezepelumab, a human monoclonal antibody that blocks the activity of thymic stromal lymphopoietin, reduced annual asthma exacerbation rates and type 2 inflammatory biomarkers in patients with severe, uncontrolled asthma, according to a recent analysis.
Jonathan Corren, MD, of the David Geffen School of Medicine at the University of California, Los Angeles, and colleagues conducted the post-hoc analysis of the multicenter, randomized, double-blind placebo-controlled phase IIb PATHWAY study. The results of the analysis were published in Allergy.
The study included adults with severe, uncontrolled asthma (n=550) who the researchers randomized to receive tezepelumab or placebo for 52 weeks (n=138). Patients treated with tezepelumab received a dose of 70 mg (n=138) or 210 mg (n=137) every 4 weeks, or a dose of 280 mg every 2 weeks (n=137). The investigators measured blood eosinophil count, fractional exhaled nitric oxide (FeNO), serum total immunoglobulin (Ig)E, interleukin (IL)-5, IL-13, periostin, thymus and activation-regulated chemokine (TARC), and thymic stromal lymphopoietin at baseline and over the course of the 52 weeks.
The annualized asthma exacerbation rate was reduced from baseline by 66% at week 52 in patients who were treated with tezepelumab versus those who received placebo.
Patients who received tezepelumab 210 mg had a greater median percentage reduction from baseline in all biomarkers at week 52 than patients who received placebo. The researchers reported that the “most notable differences” at week 52 between patients treated with tezepelumab 210 mg and those who received placebo were in the levels of IL‐5 (−60% vs 2.8%, respectively), IL‐13 (−51.6% vs −1.5%, respectively), blood eosinophil counts (−50% vs −3%, respectively), levels of FeNO (−25.2% vs 0%, respectively), serum total IgE (–20.1% vs –1.4%, respectively), and TARC (−19.0% vs −6.7%, respectively).
In patients treated with tezepelumab 210 mg, blood eosinophil counts and levels of FeNO, IL‐5, IL‐13, and periostin were reduced at week 4, while serum total IgE and TARC levels “decreased gradually until end of treatment” at week 52, the investigators reported. All biomarker reductions were maintained throughout the 52-week treatment.
The greatest reductions in biomarker levels from baseline in patients treated with any dose of tezepelumab were reported in patients who had a baseline blood eosinophil count of at least 150 cells/µl and FeNO levels of at least 25 parts per billion (ppb), followed by patients with blood eosinophil counts of at least 150 cells/µl and FeNO levels below 25 ppb.
“In conclusion, positive correlations between specific [type 2] inflammatory biomarkers that were observed at baseline demonstrate the robust relationships between several biomarkers of [type 2] inflammation,” the investigators wrote. “We have further demonstrated that tezepelumab reduces levels of inflammatory mediators, which may be reflective of decreased airway inflammation, and reduces exacerbations irrespective of baseline levels of a broad range of [type 2] inflammatory biomarkers when biomarkers were assessed individually.”
Corren J, Pham TH, Garcia Gil E, et al. Baseline type 2 biomarker levels and response to tezepelumab in severe asthma. Allergy. 2022;77(6):1786-1796. doi:10.1111/all.15197





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.