
A study published in Obstetrics & Gynecology Science found that bone mineral density (BMD) was significantly lower in women with cervical and ovarian cancer compared with healthy individuals, and BMD was particularly decreased in patients with endometrial cancer who had undergone treatment. “The risk of bone density loss and osteoporosis in gynecological cancer should be recognized, prevented, and diagnosed early to reduce the incidence of osteoporotic fractures,” the authors wrote.
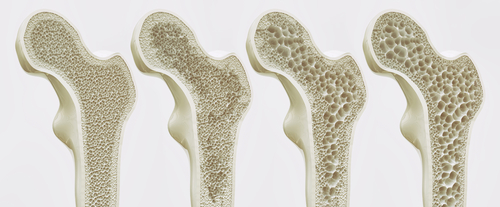
Researchers evaluated the risk of osteopenia and osteoporosis by examining the BMD of the lumbar spine and femur in patients with gynecologic cancer without bone metastasis and evaluated the impact of treatment for different cancers on BMD.
Researchers retrospectively assessed medical records of 243 women with gynecologic cancer and 240 controls (healthy post-menopausal women without gynecologic cancer) between March 2010 and December 2016. Patients with cervical cancer (n=105), endometrial cancer (n=63), and ovarian cancer (n=75) were treated with total hysterectomy, including bilateral salpingo-oophorectomy and/or chemotherapy and/or radiotherapy. All patients underwent physical examination, blood tests, ultrasonography, and BMD measurements. BMD before and after cancer treatment in patients with gynecological cancer was compared with the control group.
Before anti-cancer treatment, the BMD of patients with cervical cancer and ovarian cancer was significantly lower than that of the control group, while the BMD of patients with endometrial cancer was not significantly different from that of the controls. However, the BMD of endometrial cancer significantly decreased after treatment.
According to the treatment methods, there were significant differences in the BMD of L3, L4, and the femur neck. Changes in the BMD were lowest in patients who underwent surgical treatment only, while the highest bone loss was observed in patients who underwent postoperative concurrent chemoradiotherapy.
Among women with gynecologic cancer, 96 (39.5%) were in the normal range, 114 (46.9%) were diagnosed with osteopenia, and 33 (13.6%) were diagnosed with osteoporosis. In the control cohort, 118 participants (49.2%) were in the normal range, 100 (41.7%) were diagnosed with osteopenia, and 22 (9.2%) were diagnosed with osteoporosis. There was no significant difference between the groups (P=0.079); however, the rates of osteopenia and osteoporosis were 5.2% and 4.4%, respectively, higher in patients with cancer compared with controls.
“During the treatment of gynecologic cancer, strategies should be implemented to mitigate these risks,” the researchers concluded.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.