A study analyzed the prevalence of and risk factors for venous thromboembolism (VTE) in patients with psoriasis and psoriatic arthritis.
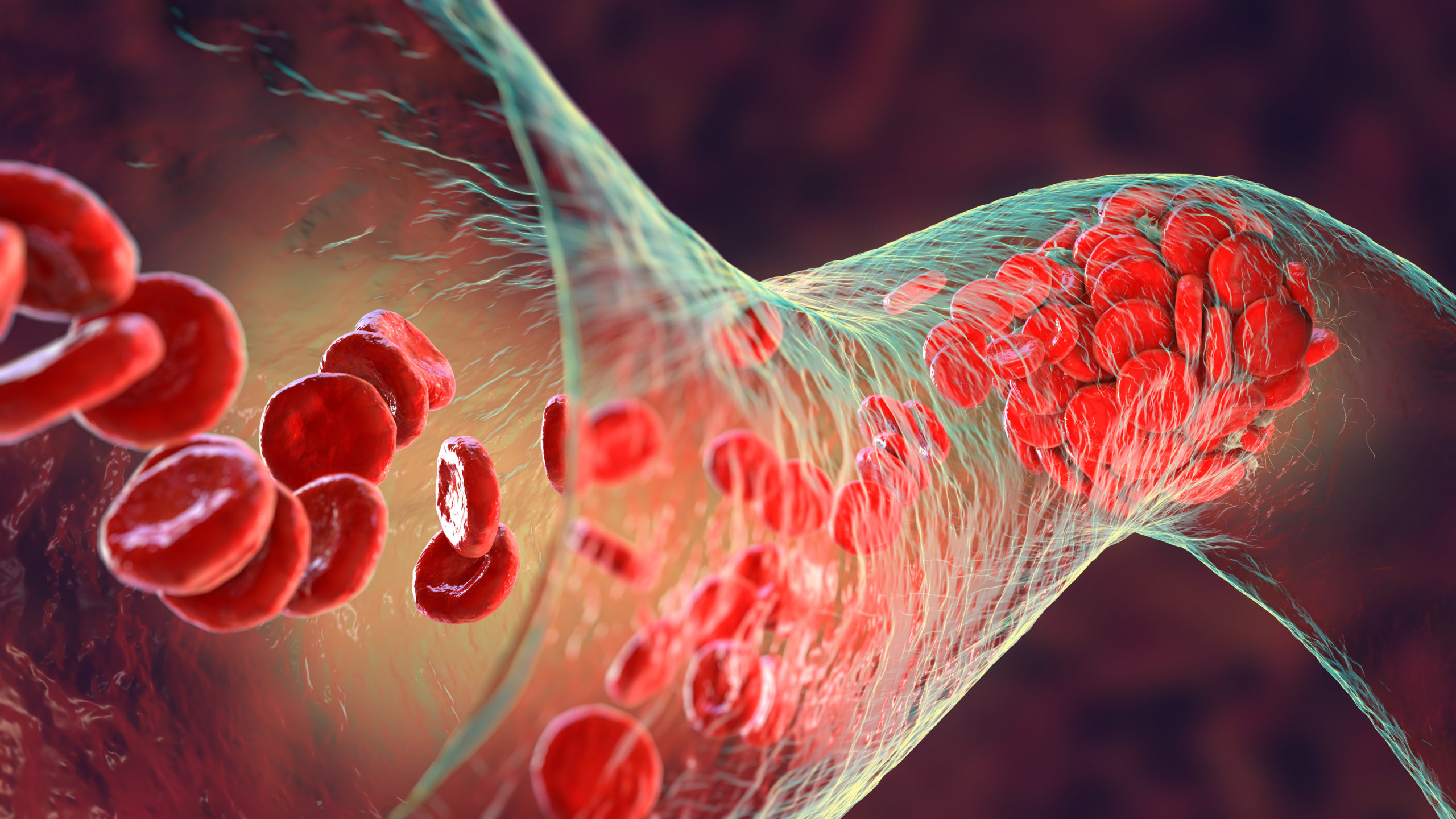
Researchers prospectively followed patients with psoriatic disease (PsD) from 1994 to 2020 and collected data on pulmonary embolism (PE) and deep venous thrombosis (DVT) using provincial hospitalization databases. They implemented Cox proportional hazards models to evaluate the correlation between comorbidities and disease-related factors and VTE.
Final analysis included 2,433 patients, and there were 26 incident VTEs, including DVT alone (n=7), PE alone (n=12), and PE and DVT (n=7). The incident rate of the first VTE was 12 events per 10,000 patient-years; the rates for DVT and PE were 6.5 and 8.8 events per 10,000 patient-years, respectively. By age 80, 4.6% of patients had developed their first VTE. Factors independently correlated with VTE were older age, diabetes mellitus, and corticosteroid usage (P<0.05 for all).
The study was published in Seminars in Arthritis and Rheumatism.
“Older patients with PsD, those with diabetes, and those using corticosteroids are at a higher risk of developing VTE. Risk stratification of patients with these identified risk factors for VTE will allow for more individualized patient management and improved medication selection,” the researchers wrote in their conclusion.
A 2014 study published in the European Heart Journal assessed the risk of VTE in patients with psoriasis and psoriatic arthritis versus controls. When adjusting for risk factors, patients with mild psoriasis were at a significantly greater risk of VTE than population controls (hazard ratio [HR], 1.07). patients with severe psoriasis and psoriatic arthritis who had a disease-modifying antirheumatic drug (DMARD) prescription had a higher risk for VTE, but this was not statistically significant. Outcomes for DVT were similar to those for VTE.
The study also assessed patients with rheumatoid arthritis (RA) and found that they were at a greater risk for VTE; this was true of both patients with and without a DMARD prescription (HRs, 1.35 and 1.29, respectively).




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.