Panelists Weigh in on Port Delivery Systems for Neovascular AMD Treatments
By DocWire News Editors - Last Updated: April 28, 2023Ehsan Rahimy, MD, moderates a discussion about hands-on experience with port delivery systems for patients with neovascular AMD.
Ehsan Rahimy: Let’s spend some time talking about port delivery. Has anyone had hands-on experience with it? How are the conversations going with your patients when you talk about this option with them?
Ali Khan: I think the conversations are tough, actually. I think partially because we now have agents that are getting out to 16 weeks. So how do you say, “Well, this is an implantable surgery and you might need a refill exchange every 6 months versus an injection every 4 months or potentially longer.” That’s a question. I think, as a clinician, I don’t have a real reason to push for one versus the other, but I do have some patients who are just so averse to injections that this comes up. And again, I think we’re still on the neovascular AMD topic, so we know that these patients tend to need anti-VEGF blockade longer than, say, a diabetic or other patients. So, in this population in particular, patients who simply are averse to having injections for whatever reason, I do bring it up.
And Diana already brought up the 3-times higher endophthalmitis rate and will that be refined lower as we have more experience surgically, which I think we already are seeing. I think it’s a hard discussion. I don’t know, if I were a patient, which one I would truly take. If I could get away with an injection every 4 months, that might convince me to stay away from, say, a surgical procedure, but I think, luckily, we’re going to let logistics work themselves out for both. How to actually get a patient into an ambulatory surgery center (ASC) to do this procedure is still not super easy, I think, financially in some places. So, I think all these other considerations might come into play more than the actual efficacy of the device or the injectable itself.
Caroline Baumal: The one thing about the port delivery system that is really interesting is that it may be something that we could give even longer durability medications via. And for that reason, I think that it’s a real unique game changer in the way that we deliver medications, to have this sort of mechanism where we can put something in and refill it and do it relatively safely, albeit the risks are higher than what we’re used to. But if we find a new medication or a different type of therapy, it holds real promise. What if we could see patients, treat patients every 1 year or every 2 years? That would really change the way that we do things.
Ehsan Rahimy: Who would be good candidates for port delivery? For those of you who are starting to have these conversations, what are you looking for to make a good candidate versus a bad candidate?
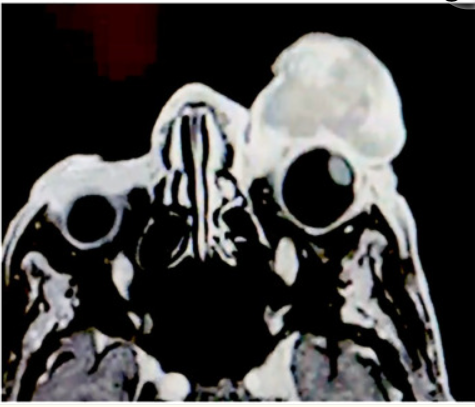
Diana Do: I think we’ve looked at patients who are optimal candidates for the port delivery system. Those would be patients who have no prior history of glaucoma surgery. They should have healthy conjunctiva, be able to follow up in case there was an adverse event. It does require going to the operating room, so they need clearance for that. I think we’ve also learned that with the port delivery system, besides the increased risk for endophthalmitis, there are other potential complications such as conjunctival erosion or even dislocation of the septum within the port delivery system, which would affect any future refills. These are all considerations that need to be taken into place before choosing a good candidate for the surgery.
Ehsan Rahimy: Any surgical tips from those who have performed the procedure? I’ve gone through the trainings. I think Genentech has actually done a wonderful job of extending a lot of virtual online education with their videos and having some of the PIs who’ve done a lot of the surgeries come out and do talks and wet labs. We had one at Stanford recently. Any surgical tips from the panelists in terms of avoiding some of the pitfalls we’ve heard about in the studies?
Caroline Baumal: I think it’s important to be very meticulous with the surgical technique. For those of us who do vitrectomy, we’re used to putting the ports in and pedal to the metal, and this is a little bit different. We have to really pay attention to the conjunctiva, do a careful dissection. And as you said, Genentech provides surgical liaisons who are able to be there and give instruction and to learn from their experience, because they really have been there and videotaped and watched so many of these surgeries. It’s not what we’re used to, having someone leaning over us, talking to us, and giving us instruction with surgery. But it’s important to, like Diana said, be careful with the conjunctiva and fill the device exactly how they say, make the incision the exact size that they say, and do the diathermy of the choroid, and follow the videos exactly to their precise instructions.
Diana Do: I think it’s also important, once you implant it, that the refill in the clinic, which occurs every 6 months, also has to be done quite precisely to avoid a dislocation of the internal septum. And the refill needle is a specially designed one that needs to be placed perpendicular to the septum to allow for the exchange and the refill of the new drug inside the device.
Ali Khan: Actually, looking at the videos, the refill procedure almost makes me more nervous than implanting the device. I feel like the videos for implanting the device are quite good now, with step-by-step instructions. The refill is the one I’m still a little bit unsure of, but I’m sure we’ll get better experience with that as well.
But what Caroline mentioned earlier about the concept of this device that’s just a reservoir for whatever you wanted to put into it, I think is just an interesting idea. Similar to, say, gene therapy, whether it’s suprachoroidal or otherwise works out, that might completely obviate this type of device. But while we’re still figuring that out, it’s certainly a new option out there. I think maybe part of my own hesitation is almost waiting to see if these other treatments that don’t require a device pan out, would that be better? And I don‘t think we‘re going to know that for a few years, but it’s certainly a good option while we’re waiting.
Ehsan Rahimy: Absolutely. This is kind of like version 1.0. It‘ll be very exciting to see where subsequent versions head.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.