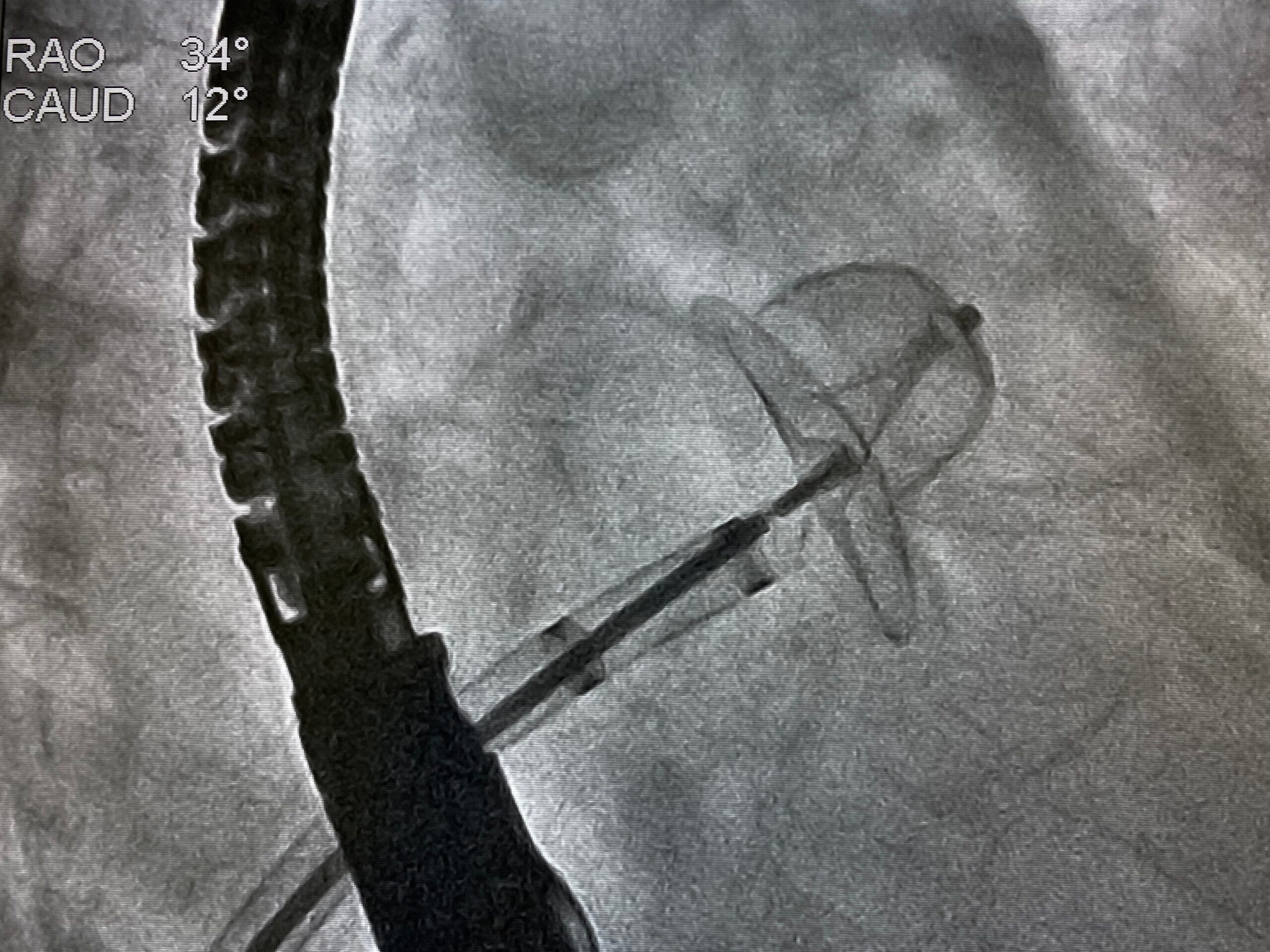
In a meta-analysis published in JACC Cardiovascular Interventions, researchers sought to investigate potential risk factors and outcomes associated with new-onset atrial fibrillation (NOAF) in patients who underwent transcatheter aortic valve replacement (TAVR). Tammy Ryan, PhD, the study’s lead author, reported that NOAF is common after TAVR, but noted that “whether AF after TAVR is a causal factor or a marker of sicker patients remains unclear.”
The systematic review included 179 studies with a total of 241,712 patients that were diagnosed with NOAF after undergoing TAVR between 2008 and 2020. Investigators used random effects model to pool the collected data.
According to the article, the pooled occurrence of NOAF after TAVR was 9.9% (95% confidence interval [CI], 8.1–12%). The presence of NOAF after TAVR was associated with a longer hospitalization index (mean difference = 2.66 days; 95% CI, 1.05–4.27), a higher stroke risk in the first 30 days (risk ratio [RR] = 2.35; 95% CI, 2.12–2.61), 30-day mortality (RR = 1.76; 95% CI, 1.12–2.76), major bleeding (RR = 1.60; 95% CI, 1.39–1.84), and permanent pacemaker implantation (RR = 1.12; 95% CI, 1.05–1.18). Furthermore, the risk factors for NOAF after TAVR included higher Society of Thoracic Surgeons scores, transapical access, pulmonary hypertension, chronic kidney disease, peripheral vascular disease, and severe mitral regurgitation, “suggesting that the risk for NOAF is highest in more comorbid TAVR patients,” the authors commented.
Overall, the authors could only conclude that NOAF was frequent in patient who underwent TAVR and did not find conclusive evidence for factors that could effectively predict NOAF risk.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.