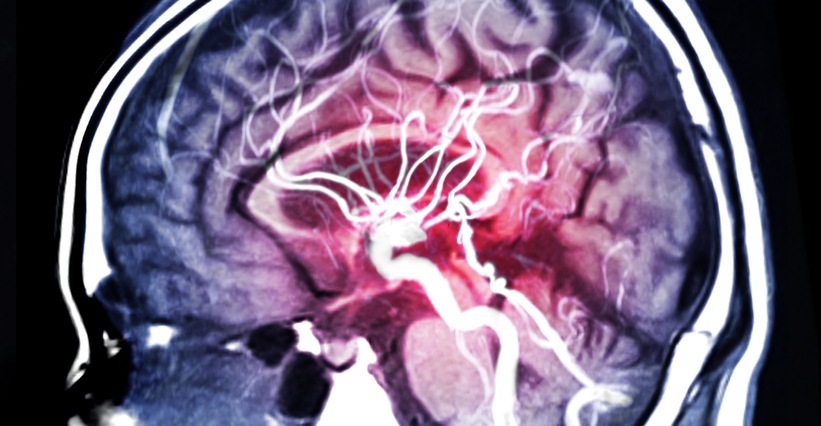
A study presented at the CHEST Annual Meeting 2020 assessed the prevalence of sleep disordered breathing (SDB) among patients following intracerebral hemorrhage (ICH) and the mean apnea-hypopnea index (AHI).
Researchers queried PubMed, Scopus, CINAHL, and clinicaltrials.gov for relevant studies published through April 1, as well as performed a manual references review. Eligible studies reporting the prevalence of SDB after ICH and mean AHI that used an American Association of Sleep Medicine (AASM) type 1-4 sleep study device (SSD) were eligible for inclusion. Studies were excluded if SDB prevalence in ICH survivors was not available, could not be determined, or was evaluated in a way not utilizing an AASM SSD. AHI was used to determine the prevalence of SDB. A random-effects model was implemented to determine weighted averages with 95% confidence intervals (CIs) per SDB by AHI cutoff: >5, >10, >15, >20, >30, and >40.
The researchers identified 120 full texts, of which 17 studies encompassing 496 total patients were included in the final analysis; study heterogeneity ranged from low to high. SDB prevalence in ICH survivors per AHI was: >5, 82% (95% CI, 74-88); >10, 61% (95% CI, 54-68); >15, 50% (95% CI, 42-57); >20, 37% (95% CI, 30-45); >30, 23% (95% CI, 17-30); and >40, 15% (95% CI, 4-47). Overall, the mean AHI was 19.08.
“Due to the high morbidity and mortality, many ICH survivors do not get screened for SDB or cannot tolerate testing. SDB prevalence may vary in ICH survivors in accordance to genetic, social, and pathological factors. Implementation of a feasible protocol with uniform methodology and further prospective trials are needed for more conclusive data,” the study authors concluded.







 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.