Infectious Disease Specialist: Vaccinated People May Not Need to Mask, Distance Around Others Who are Vaccinated
By Kerri Fitzgerald - Last Updated: February 10, 2021Payal Kohli, MD, FACC, DocWire News Medical Lead and Section Editor, recently spoke with Monica Gandhi, MD, MPH, an infectious disease doctor from the University of California, San Francisco, about available phase III data for six COVID-19 vaccines, how the vaccine rollout can be improved, when we can “return to normal,” and more.
Dr. Kohli: Hello, and welcome to DocWire. My name is Dr. Payal Kohli. I’m a cardiologist from Denver, Colorado, and editor of the cardiology section at DocWire. It’s my pleasure today to be joined by Dr. Monica Gandhi. Dr. Gandhi is an infectious disease doctor, a professor of medicine, and associate chief in the division of HIV, infectious diseases, and global medicine at the University of California, San Francisco.
We’re very excited to have you here today because you’ve obviously done a lot of impactful work in COVID-19 in mitigation strategies. But I really want today to focus on our discussion about vaccines and how they’re going to change the face of the pandemic.
I want to start just by asking you to talk a little bit about the available vaccines that are out there, what’s cooking on the horizon, and how you think they’re going to impact our fight against this virus.
Dr. Gandhi: It’s great news that we actually have six phase III trial results now for six different vaccines. In fact, just this morning, it looks like there’s going to be some data coming out of the vaccine from China.
At this moment, we have four full publications for the Moderna vaccine, the Pfizer vaccine—which are both mRNA vaccines—then we have the Johnson & Johnson vaccine, which is not yet in publication, it’s a adenovirus DNA vaccine; and then we have Novavax, which is a protein vaccine with an adjuvant, which is also not yet released; then we have the Sputnik V, which is adenovirus vaccine which is in publication form; and then we have the AstraZeneca-University of Oxford vaccine and Novartis DNA.
We have six vaccine phase III trial results, so that is really exciting to have that this early after the pandemic.
Dr. Kohli: There’s obviously advantages and disadvantages of each candidate’s availability, but in general, what would your advice be for us to tell our patients when they ask us, “Which vaccine should they get?”
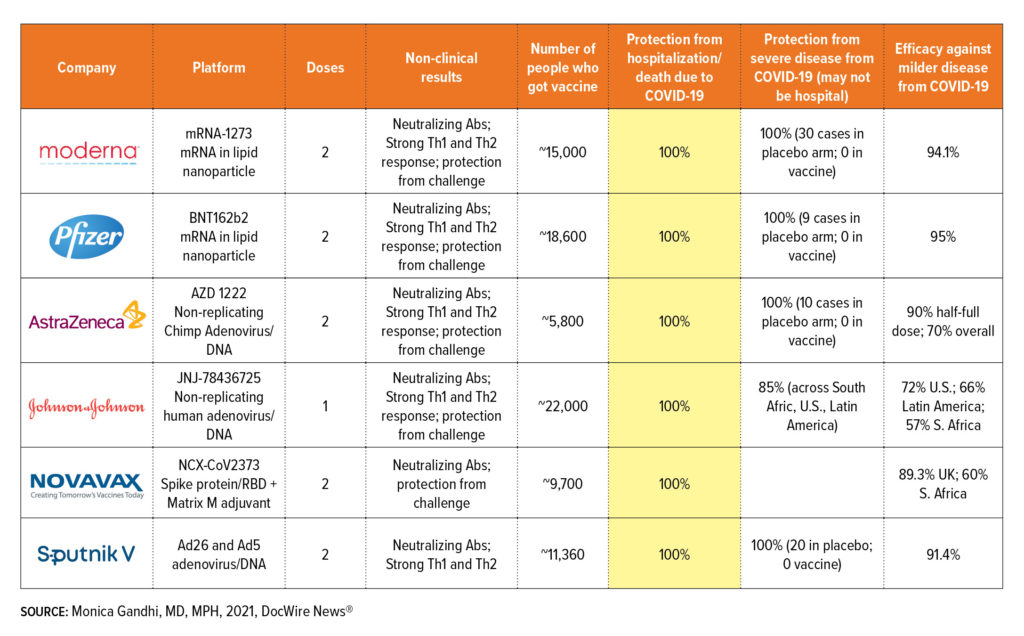
Dr. Gandhi: Right now, only Moderna and Pfizer are authorized in the U.S., but the Johnson & Johnson vaccine, its FDA Emergency Use Authorization date is February 26, and we do expect to hear favorable results from that. If that’s true, there will truly, in a way, be a choice, or I don’t know if there’s a choice, but there’ll be a discussion to be had with patients because right now, Moderna and Pfizer are pretty much the same thing. mRNA vaccines work great—95% efficacy, 100% against severe disease. The Johnson & Johnson vaccine is different. It’s an adenovirus. It has DNA in it. It’s kind of more traditional of a vaccine, and it was really effective. Again, it prevented hospitalizations at 100%, and we have a table here that shows this, but its efficacy against mild disease was a little less than the mRNA vaccine, so let’s focus on severe first.
There is a category called severe disease, which they didn’t define that well because it’s in the press release. We really need to see that FDA briefing that they’ll put out, but it was 85% effective against severe disease, which included the subset of people who are hospitalized. It was equally as effective for severe disease in the U.S., in South Africa, in Latin America, and in the South Africa site, they actually sequenced the virus and said 95% of the circulating virus was the B1.351, the South Africa variant. So really great efficacy, same efficacy even against that variant for severe disease.
It was mild disease where the Johnson & Johnson differed. It prevented mild disease at 72% in the U.S. and 57% in South Africa. This could be that T-cells help us mediate responses to severe disease, and the T-cells are great, but maybe our antibodies are not as robust against the South Africa variant with Johnson & Johnson. Given that we don’t need to be perfect, given that this is really effective in the U.S., given that severe disease is averted at that high rate, and given we don’t have great vaccine rollout yet because of the Moderna and Pfizer, we don’t have the supplies, I would favor, and I hope the FDA will approve it, authorize it. I do think that patients should feel comfortable that they’re getting the percent efficacy that we were dreaming of in the summer. We used to say, “Oh, 60%. That would be amazing.” We got spoiled a little with the 95% with the mRNAs.
Dr. Kohli: All great points. It also raises, obviously, the issue of the one dose vaccine versus requiring two doses and which one is going to get us to our target faster. I’m curious which side of the coin you fall on. Some health experts have said it makes more sense, even with the Moderna and Pfizer vaccine, to get those first doses out, delay those second doses, and just try to get as many people getting the first dose. Others have said the opposite, like Dr. Fauci, which is that we really need to stick with the timeline. What are your thoughts on which of those we should be employing as a country?
Dr. Gandhi: I do have an opinion on that. I will say you’re right, absolutely, the Johnson & Johnson… you’re so right to say, “One dose. How great.” That will make it easier, but in terms of the one dose versus delaying the second dose versus doing the two doses on schedule for the mRNA vaccines, I fall on the side of one dose to everyone now and delaying the second dose. In no way, I don’t think anyone’s ever written, except for maybe people who have had COVID-19 before, which is a whole other dataset, that anyone should not get the second dose. The second dose has to be given.
But there’s lots of reasons in my mind why we could delay the second dose to get to herd immunity faster, to get people partially vaccinated faster. One is that the AstraZeneca trial showed, which is a different vaccine, that the longer you wait between doses, the better. Actually waiting 12 weeks was better than nine weeks was better than six weeks.
That was helpful information that delaying is okay. Second, is that actually, when we think about childhood vaccinations, we don’t care if a child comes in too late. We care if a child comes in too soon, and if they come in too soon, we won’t give the second dose, but a child that comes in late, you don’t restart the vaccine series. You just give the vaccine because there’s this principle in vaccinology that waiting between doses is not going to hurt anything. In fact, it could be more efficacious.
Third, the phase I, phase II data of the mRNA vaccine showed immunogenicity was increasing after the first dose. The reason they did three to four weeks for the second dose is because they were in a hurry for these trials.
I see no problem delaying the second dose, and I do differ from others on that. I don’t think it’s like antibiotics. I don’t think you’re going to break through with mutant virus.
Dr. Kohli: Those are all great points. Now you mentioned herd immunity. We talk about this virus having a herd immunity threshold of about 70%. When do you think we’ll get to that, urrently, based on how the rollout is going, and how do you think our lives will be once we get there? Do you think we’ll be wearing these masks forever? Do you think there’ll be some semblance of normalcy in our lives after we cross that threshold?
Dr. Gandhi: Yes. I actually am of very much of the ilk that we will get back to normal. We will not mask in distance. In fact, if anything has revealed how loneliness and mental health and how important it is for primates like humans to be together, it has been this pandemic. I would really encourage policymakers to think about the impact of loneliness during this pandemic.
I do believe herd immunity is going to be 70%. Like you say, it all depends on the vaccine rollout progress. The way we’re going now, we’re not going to get there, I think, unless we get the Johnson & Johnson vaccine, or unless there’s some magical uptick in the Moderna and Pfizer, which they are saying they’ll get more of the doses in March.
The reason I say that is, California has been given best estimates of 1 million doses a week. That’s best estimate. That would be 40 weeks to get to 40 million people. If we have the Johnson & Johnson, I think we could get there by fall. If we don’t get the Johnson & Johnson, which I hope we do, I think we’re not going to get there till winter of 2021.
It will be obvious when we get to herd immunity. It’s not like people are going to be counting the number of people and say, “This is the tick mark of 70%.” What will be obvious is that hospitalizations will decrease massively like they are with real-world rollout programs in Israel. They will decrease massively. We will see it.
Second is that people will be swabbing for cases because they do swab, and we test very frequently, and those cases will be coming down. It will reveal itself almost that it simply won’t be the health problem of the day. That’s the magical thing about herd immunity. The virus can’t find anyone to infect. I’m very hopeful for fall if we can get the Johnson & Johnson.
Dr. Kohli: We’ve already vaccinated a lot of healthcare workers, obviously nursing home residents. There was some debate about whether we were starting in the right population because this is not the population that’s most likely to be spreading the virus. It’s more the younger individuals, but we’ve received some data that the vaccinations thus far have already started to make an impact on hospital morbidity and mortality. What are your thoughts on that? Do you think we’ve already started to make a dent in the impact from this pandemic with the vaccines we’ve administered thus far?
Dr. Gandhi: That’s a great question because the Centers for Disease Control and Prevention (CDC) on February 7 estimated we reached 32 million Americans, which is 10% of the population. There is also an estimate from the same body that maybe 30 million people or more, maybe even more, Dr. Offit has gone up to a third of the U.S. population has been already infected with COVID-19. Unclear where exactly where we stand. What is that exact number? We won’t know because we haven’t done massive serology studies, but between our natural immunity and the vaccine rollout and, of course, likely, all the restrictions which are still ongoing, there’s no doubt our hospitalization rates are down, which is great news. We should be celebrating this massively. Yes, I kind of think the vaccinations are contributing because North Dakota and West Virginia are the two places where they’ve had the best rollout, uniquely. New York and California have been on unfortunately behind, and they are seeing no deaths over days, for example, from COVID-19. It’s really reassuring to see the vaccines do what they’re supposed to do.
Dr. Kohli: Now that we know the vaccines offer partial protection, at least, against the new variants, we did get some disturbing news out of South Africa, obviously, about the AstraZeneca vaccine not reducing mild to moderate illness in the South African variant, but I’m curious, what sort of precautions do you think we ought to continue to exercise even after we’re vaccinated as healthcare workers? Are you double-masking? Are you continuing to socially distance? What advice would you give your colleagues and your friends?
Dr. Gandhi: I do think the CDC is going to update their advice on this based on something Dr. Fauci intimated in a press conference. I think two vaccinated people can be together without restriction. I think we’ve been messaging so far that nothing changes after vaccination. I think that is actually pretty discouraging to people because what is the point? We know these vaccines will get us out of it. I’m all for tiered, nuanced messaging because I’m an HIV doctor at heart. I don’t say to my patients who don’t have HIV, “This is what you have to do even if your partner’s positive or negative.” It’s like very nuanced. I’m saying two positive people, this is my recommendation. Two people who, one person who doesn’t have HIV, one person who does have HIV, this is my recommendation. It’s called tiered messaging.
I would recommend that vaccinated people do not maintain these restrictions of masking and distancing. This has implications for people in a hospital setting, healthcare workers going back to in-person meetings, because I think teaching rounds, clinical care, there’s a lot that’s been affected in our own system by the restrictions. Theoretically, and I do believe that we should still message this, a vaccinated person being out in society because we don’t have mass vaccination yet has to behave as if they’re protecting others. They have to mask and distance, so that they go to the store, mask and distance because there’s no letter that says if you’re vaccinated or not.
The third is a vaccinated person against an unvaccinated person, one-on-one, should protect that unvaccinated person by masking and distancing one-on-one, like a doctor with a patient. Now, do I think that these vaccines are going to decrease asymptomatic infection? I do. This is the most prudent recommendation at the time.
Dr. Kohli: I really like that tiered approach because I think you’re right. One of the ways that we’re going to get mass vaccination out there is to really motivate people that it is going to allow us to get our lives back to normal. The message has just been everybody keeps doing the same thing because some of those subtleties sometimes get lost on people.
We did get some encouraging data about the Pfizer vaccine today that maybe it does reduce transmission as well. Of course, we’ve seen that both with Moderna and with the AstraZeneca vaccine, asymptomatic infection is reduced as well. I think you’re absolutely right that once all of us are vaccinated, our lives will get back to normal. But in the meantime, for those of us that are vaccinated, we can perhaps start to think about relaxing some of those restrictions, which I think will be welcomed change for all of us.
Dr. Gandhi: And good for mental health.
Dr. Kohli: That’s exactly right. And substance use and all the other things that have really been collateral damage from this pandemic so far.
Dr. Gandhi: Definitely.
Dr. Kohli: My last question for you, Dr. Gandhi, is what do you really think about how the COVID-19 vaccine rollout has been going? What would you do differently? And you did allude to some states that had done it right. Do you think there ought to be some sort of federally guided COVID-19 rollout? We’ve still got several months ahead of us getting this vaccine out. What would your advice be if you were sitting on President Biden’s taskforce?
Dr. Gandhi: My advice would be very specific around that, actually. I really liked when the Advisory Committee on Immunization Practices could put out their guidelines in December about tiered rollout because it just totally made sense to me. First, healthcare workers and long-term care facilities, then older people, then essential workers in different tiers. It actually ended up being a barrier because keeping a strict adherence to tiers, which California has done for example, has meant, and I’m in a hospital on the ground trying to volunteer for vaccination shifts, and they don’t need me because it’s right now only above 65 years. At our hospital, we serve a vulnerable patient population. They don’t all have phones. We can’t find all the 65-year-olds. In the meantime, children can’t go back to school because teachers are asking to be vaccinated first.
I would first collapse it from the federal government. I would give this advice that says immediately, over 65 years and essential workers, and I would go so far as to 16 to 64 years with medical conditions. Not because we have all those vaccine supplies, but the very barriers that we set up means that at the end of the day, vaccines can go to waste. We can’t slot people in if someone doesn’t show up for their appointment. Any logistical barrier you can decrease, which is what West Virginia, North Dakota, Texas, and many places have done has actually ended up doing better. It’s true they don’t have enough supply, but whatever supply they have goes right into people, whereas we’re still sitting on supply in California, which is sticking with the greater than 65 years.
I’m very concerned about teachers and schools and teachers on needing to go back into classrooms. I would at least open it up to essential workers and over 65 years.
Dr. Kohli: I really like that because you’re absolutely right. We’re actually creating those bottlenecks by having this tiered system. Then of course, the supply is a bottleneck as is the administration, but those are natural bottlenecks we can deal with. The tiered system, in some ways, has created certain bottlenecks that I do think that would eliminate.
Dr. Gandhi: We created it.
Dr. Kohli: That’s right. I want to thank you so much, Dr. Gandhi, for your time, all your wonderful insights and comments. I’ve learned so much just from listening to you and talking with you. I hope we can have another discussion very soon in a few weeks about the rest of the new mutants and the rest of the COVID-19 pandemic fight.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.