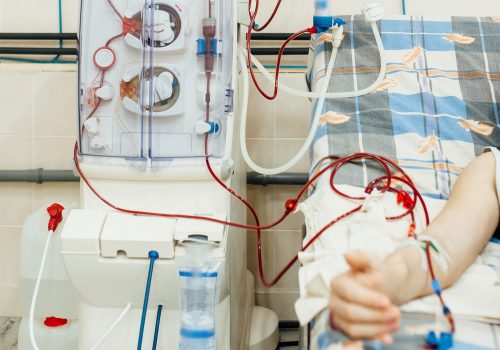
Guidelines from Kidney Disease Improving Global Outcomes recommend that all patients with end-stage renal disease (ESRD) receiving dialysis use a fistula for access. More than 90-day catheter rate prevalence at dialysis centers are tracked by the Centers for Medicare & Medicaid (CMS). The Veterans Health Administration (VA) is not required to abide by CMS guidelines; however, the VA uses them for guidance, resulting in expected rates of catheter use of less than 12.1%.
Sylvester Barnes, MD, reported on a VA quality improvement project at the NKF Spring Clinical Meetings in a presentation titled Dialysis CVC Improvement Rate: A VA Quality Improvement Project. The project was conducted at the Hines VA (HVA) hospital. Approximately 85 patients receive regular hemodialysis at HVA at the outpatient dialysis unit. In 2018, the 90-day catheter prevalence rate was above 35% consistently, far above the goals of the VA.
In response to the consistently high rate of catheter use, HVA established a multidisciplinary committee that included the dialysis attending rounding for that month, vascular surgery, and interventional radiology. New hires included a dedicated dialysis access nurse and an interventional nephrologist. The committee met biweekly and discussed in detail each patient with a catheter for dialysis access. A personalized access plan was created for each patient.
Following access creation, regular interventions were scheduled to manage access-related maturation issues, identified by routine surveillance. Following two weeks of stable access cannulation, catheters were removed. The committee met to discuss any patient with arteriovenous fistula or arteriovenous graft access who required more than one intervention in 90 days or was on the verge of failure (based on interventional nephrology or interventional radiology opinion). Those patients were placed on an unstable access list.
With the project in place, as of September 2019, the more than 90-day catheter rate decreased to 13%; projections for October 2019 indicated the rate would be less than 12%, in accordance with VA guidelines.
The authors said, “It is felt that the two biggest factors that have helped our catheter rate include forming our multidisciplinary committee, interventional nephrology hires to help provide more endovascular procedure access time, and the hiring of a dedicated access advanced nurse practitioner to help identify access-related problems and regularly schedule these patients for intervention with interventional nephrology, interventional radiology, or referral for surgical revision of the access.”
Source: Barnes S, Wadhwa A. Dialysis CVC improvement rate: a VA quality improvement project. Abstract of a presentation at the National Kidney Foundation 2020 Spring Clinical Meetings; abstract #302.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.