Time-limited treatment with bendamustine, rituximab, and venetoclax was associated with high rates of undetectable minimal residual disease (MRD) remission in a phase II study of adults with untreated chronic lymphocytic leukemia (CLL). These data were presented at the 63rd American Society of Hematology (ASH) Annual Meeting & Exhibition.
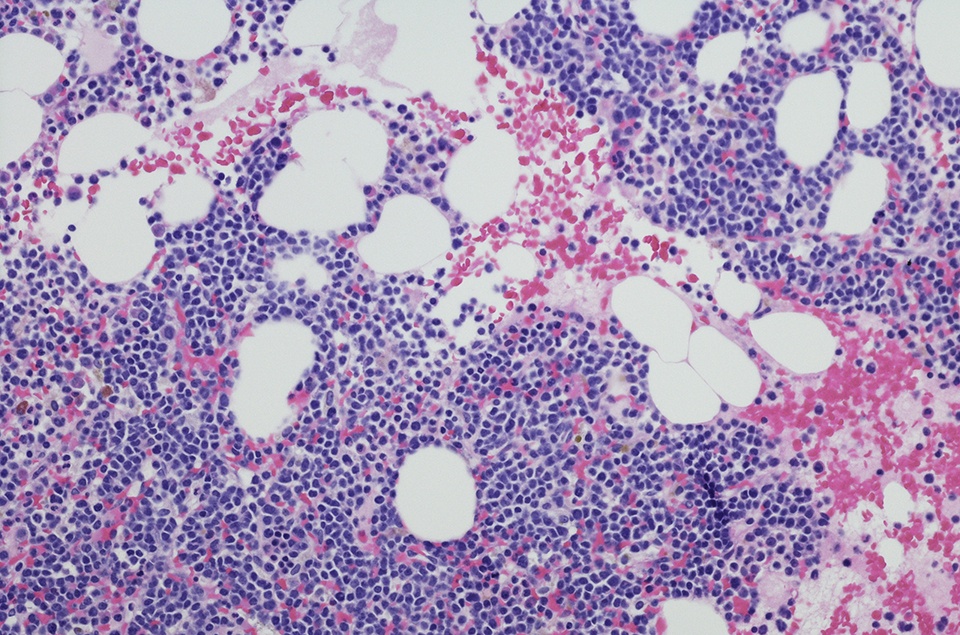
At data cut-off, 26 patients were enrolled, with ongoing recruitment. Patients received three cycles of induction with bendamustine and rituximab (BR) followed by consolidation with venetoclax and rituximab (VR) for a fixed one-year duration. During induction, patients received bendamustine 50 to 90 mg/m2 for two days and rituximab 375 mg/m2 once per 28-day cycle. Consolidation with venetoclax was initiated at 20 mg and escalated to 400 mg daily over five weeks, followed by six cycles of VR and then five cycles of venetoclax alone.
Patients were aged a median of 60 years (range = 44-77 years), and the cohort was 61.5% male. Twenty-three patients remained on the study at a median follow-up of 12.9 months (range = 1.9-27.5), including 12 patients with at least 15 months of follow-up. The overall response rate (ORR) among these 12 patients was 100%, with 92% achieving a complete response (CR; with or without incomplete count recovery) and 8% with a partial response (PR). Three patients died on study: two deaths were related to COVID-19, and one patient developed newly metastatic squamous cell carcinoma and was taken off the study following a CR during consolidation. A response assessment in 20 patients following induction showed a 15% CR rate and an 85% PR rate after BR treatment.
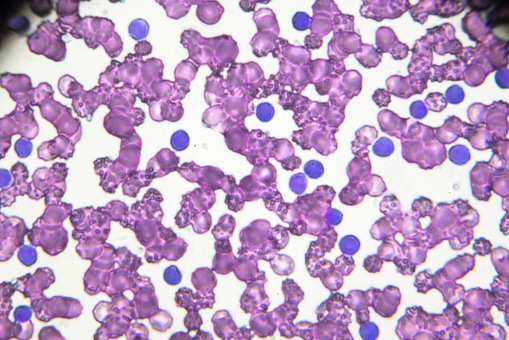
MRD evaluations in 10 patients evaluable at 16 months found undetectable MRD (<0.01%) status in 100% of peripheral blood samples and 90% of bone marrow samples. Median time to undetectable status was 12 months (range = 3-15 months) in peripheral blood and 14 months (range = 5.5-15 months) in bone marrow.
During BR induction, the most common treatment-emergent adverse events (AEs) were anemia (any grade, 21%; grade ≥3, 7%), nausea (21%; 0%), neutropenia (18%; 7%), rash (18%; 0%), constipation (14%; 0%), and transaminitis (11%; 0%). Two patients (7%) developed febrile neutropenia. Treatment-emergent AEs with venetoclax treatment included diarrhea (any grade, 36%; grade ≥3, 0%), neutropenia (21%; 11%), leukopenia (18%; 7%), and nausea (14%; 0%).
The authors noted that risk of tumor lysis syndrome (TLS) was substantially reduced after induction, with a 94% reduction of risk among patients at high or medium risk of TLS at baseline. “Of three high-risk patients at baseline, none remained high-risk after BR,” they reported. Also, “of 15 medium-risk patients, only one remained medium-risk, with the remainder at low-risk.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.