In a study of patients with cardiac amyloidosis (CA), incidence rates of arterial thromboembolic events (AEs) were high, even among those treated with anticoagulation therapy.
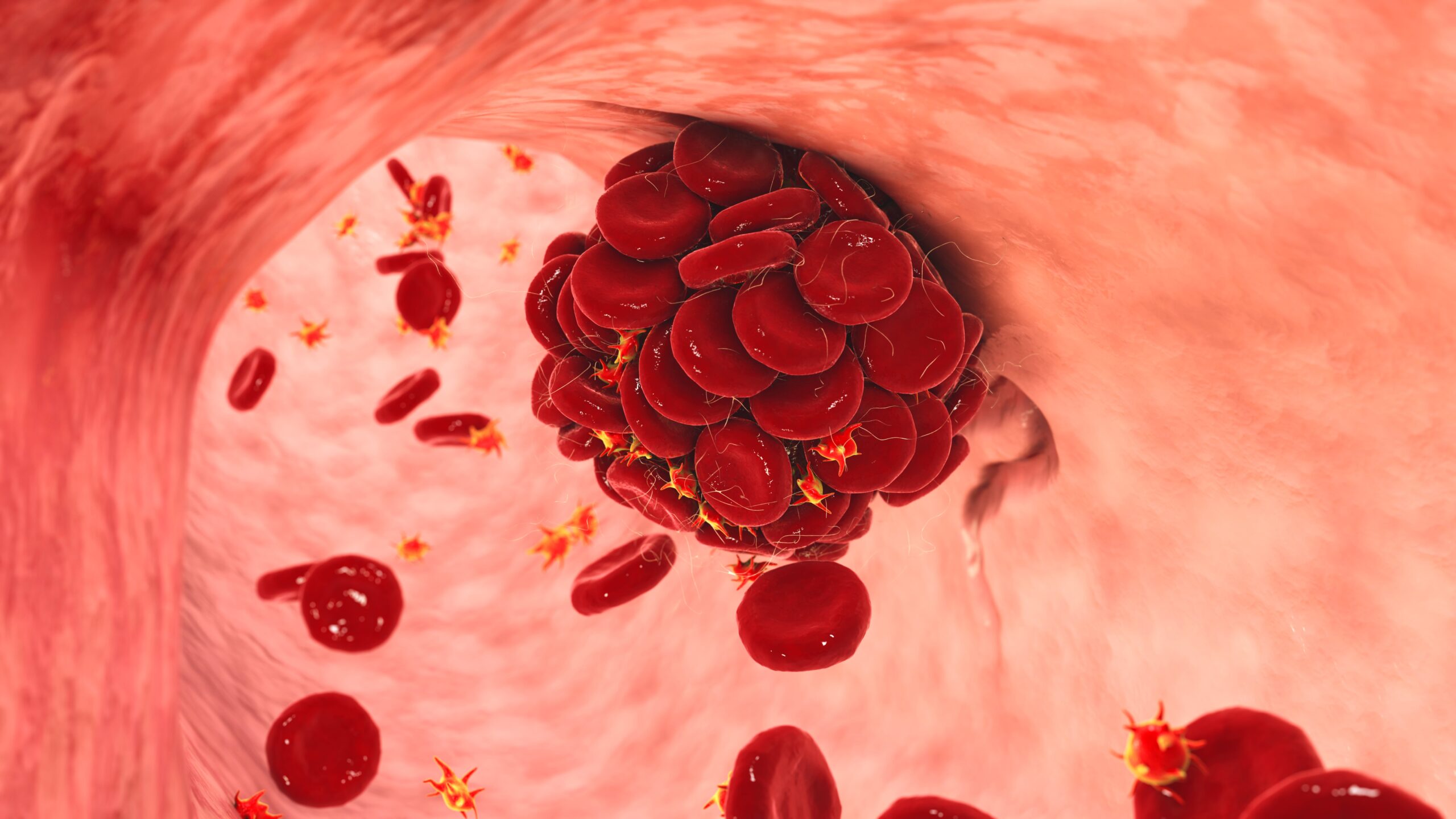
CA is the most common type of restrictive cardiomyopathy and occurs when amyloid deposits replace normal heart muscle. Arterial thromboembolism occurs due to obstruction of a normal artery by the presence of a thrombus dislodged from the site of arterial obstruction. Intracardiac thrombosis is frequently reported in CA, but data on AE frequency in CA are limited.
Researchers in Italy aimed to assess prevalence, clinical characteristics, and predictors of AEs in a large multicenter study of patients with CA. The study enrolled 406 patients across five centers, including 134 patients with light-chain amyloidosis, 73 with mutant transthyretin amyloidosis, and 199 with wild-type transthyretin amyloidosis.
In total, 31 patients (7.6%) suffered from an AE, of whom 10 (32.2%) were in sinus rhythm and had no history of arterial fibrillation (AF). There were no significant differences in age, gender, or type of CA between patients with or without AEs. Fourteen (7.6%) of 185 patients receiving anticoagulation experienced an AE despite treatment. Anticoagulation therapy did not fully protect patients from the risk of events (hazard ration [HR], 1.23; 95% confidence interval [CI], 0.52-2.92; P=0.64).
A CHA2DS2-VASc score ≥3 was the only distinguished predictor of AE, particularly among patients in sinus rhythm (overall population HR, 2.84; 95% CI, 1.02-7.92; P=0.05; sinus rhythm HR, 10.13; 95% CI, 1.12-91.19; P=0.04).
“In our large, multicentric, real-world cohort, prevalence and incidence rate of AEs was high. A consistent proportion of events occurred despite anticoagulation therapy or in patients in sinus rhythm. A higher CHA2DS2-VASc score might identify patients at risk of AEs also among those in sinus rhythm,” the authors concluded.
Findings from this study were published in Amyloid.



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.