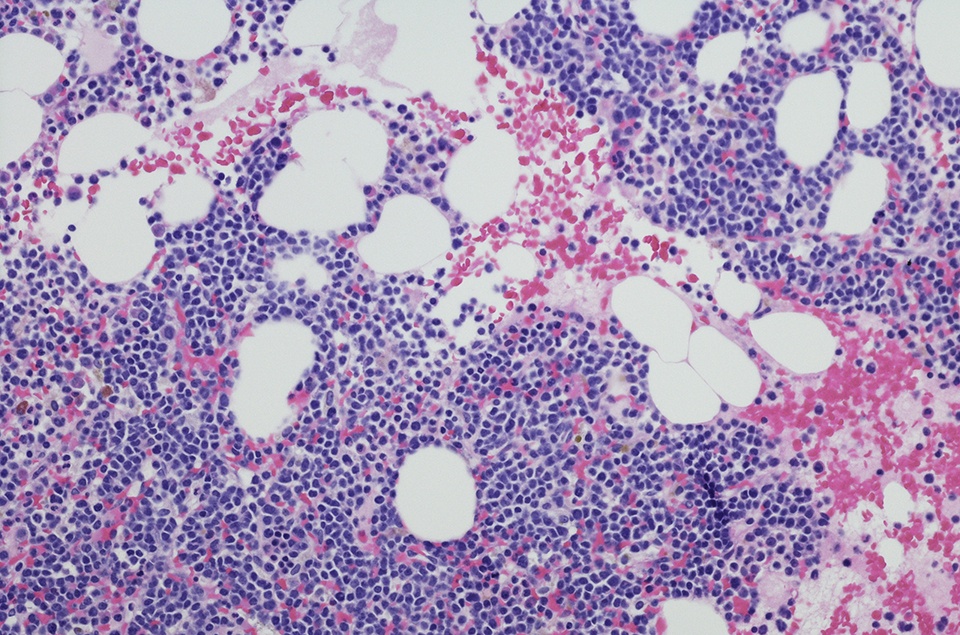
According to results from a phase I/II study, more than 90% of older and high-risk patients with newly diagnosed acute myeloid leukemia (AML) had a complete response (CR) following treatment with magrolimab and venetoclax plus azacitidine. The findings were presented at the 2021 ASH Annual Meeting.
Per the study investigators, most patients with AML experience relapse despite high response rates to front-line treatment with azacitidine and venetoclax. In the phase I portion of this study, they assessed whether the addition of magrolimab to azacitidine and venetoclax in adults with AML could improve disease outcomes.
Only patients with relapsed/refractory AML were enrolled in this phase of the study. After establishing the recommended phase II dose, an expanded protocol allowed for the enrollment of frontline, venetoclax-naïve, and venetoclax-exposed patients with relapsed/refractory AML. Patients in the front-line cohort were 75 years or older, had comorbidities that made them ineligible for intensive therapy, or had adverse-risk karyotype and/or TP53 mutation regardless of age/fitness.
Each four-week treatment cycle consisted of azacitidine 75 mg/m2 (days 1-7) and venetoclax 400 mg (days 1-28). Magrolimab was dosed on days 1, 4, 8, 11, 15, and 22 of cycle 1. Additionally, magrolimab was dosed weekly in cycle 2, then every two weeks in cycle 3 onward. There were no dose-limiting toxicities at the end of the phase Ib portion of the study, which enrolled six patients. The established recommended phase II doses of magrolimab were 1 mg/kg on days 1 and 4 of cycle 1; 15 mg/kg on day 8 of cycle 1; and 30 mg/kg on day 11 of cycle 1.
For the phase II portion of the study, the investigators focused on assessing the triplet combination’s safety and maximum tolerated dose (MTD). Secondary objectives were the rates of complete response (CR)/CR with incomplete hematologic recovery (CRi), duration of response (DOR), and overall survival (OS).
Overall, the study included 38 participants: 17 newly diagnosed patients with AML, eight venetoclax-naïve patients with relapsed/refractory disease, and 13 patients with relapsed/refractory AML who experienced treatment failure with venetoclax. The median age of the newly diagnosed patients was 70 years and ranged between 33 to 84 years. Most patients had high-risk features, including 82% who were categorized as European LeukemiaNet adverse-risk, 45% who had Eastern Cooperative Oncology Group performance status of 2 or greater, and 47% who had TP53 mutation.
In 15 of 16 newly diagnosed patients, the CR/CRi rate was 94%, and the eight-week mortality was 0. All patients had a response after the first cycle. Among the patients with CR/CRi, the median time to absolute neutrophil count recovery >0.5 was 28 days, and the median time to platelet recovery >50×109/L was 24 days.
The eight-week mortality rate among all 38 patients was 9.7%, and all deaths occurred in patients with relapsed/refractory disease. The most frequent treatment-emergent non-hematologic adverse events (AEs) included hypokalemia (58%), hypophosphatemia (55%), hyperbilirubinemia (53%), hyponatremia (53%). and sinus tachycardia (47%). Grade 3/4 AEs included pneumonia (32%), febrile neutropenia (32%), hyperbilirubinemia (11%), elevated ALT (11), and skin infection (11%).




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.