
At the 2021 American Society of Hematology (ASH) Annual Meeting, researchers presented long-term follow-up data from a phase II trial of rituximab plus bendamustine and cytarabine (R-BAC) in elderly patients with newly diagnosed mantle cell lymphoma (MCL). The results were shared by lead author Maria Chiara Tisi, MD, of the San Bortolo Hospital in Vicenza, Italy.
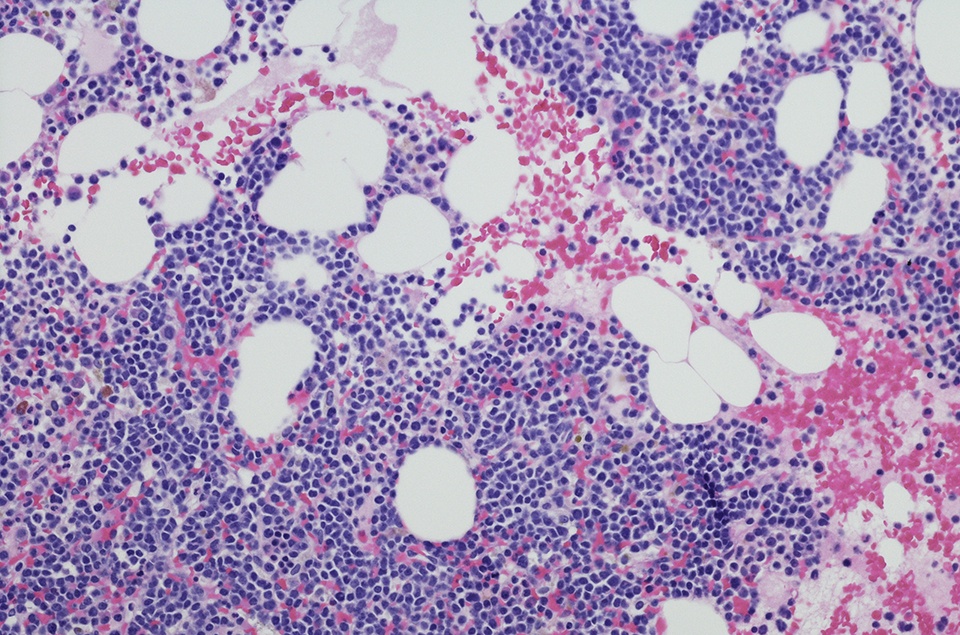
The original Italian Lymphoma Foundation trial enrolled 57 patients who were aged a median of 71 years (range = 61-79 years) with treatment-naïve MCL who were not eligible to undergo stem cell transplantation (SCT). Per study protocol, patients received four to six cycles of R-BAC between 2012 and 2014. Maintenance treatment was not planned after induction therapy, and no patient in the study received rituximab maintenance. After two-year follow-up, researchers reported that the R-BAC regimen was associated with a high complete remission (CR) rate, at 91%. The two-year overall survival (OS) and progression-free survival (PFS) rates were also high, at 86% and 81%, respectively.
In the present study, investigators presented follow-up data from a median follow-up of seven years (86 months; range = 57-107 months). Median OS and PFS were not yet met for all patients, and rates of OS and PFS were 56% and 63%, respectively. The researchers noted that the PFS rate was 59% among patients who achieved a CR at two years, “with the curve that appears to plateau after six years,” they commented. Factors that were predictive for lower PFS included blastoid morphology (P < 0.05), elevated Ki67 (>30%; P < 0.05), and failure to achieve a CR after two treatment cycles (P = 0.03). Additionally, disease progression within 24 months of initiating R-BAC was also associated with reduced overall survival (P < 0.05). Eight patients (14%) developed a secondary neoplasia.
At the ASH Annual Meeting, researchers also presented long-term measurable residual disease (MRD) outcomes from 31 patients with molecular markers at diagnosis and follow-up. MRD persistence (in peripheral blood or bone marrow) at the end of induction therapy was associated with significantly impaired seven-year PFS (all P < 0.05).
“In elderly patients with newly diagnosed MCL, R-BAC showed sustained efficacy over time, which compared favorably with any other reported immuno-chemotherapy regimen (with or without maintenance) in similar populations,” the authors concluded. “With a median OS exceeding 60% after seven years, this regimen has significantly impacted on the life expectancy of elderly patients with MCL.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.