At the Fourth Annual National General Medical Oncology Summit held in Miami, Florida, host Neil Love, MD, president and CEO of Research to Practice, moderated an expert panel on systemic mastocytosis and myelofibrosis. The panel consisted of Prithviraj Bose, MD, of MD Anderson Cancer Center, Andrew Kuykendall, MD, of Moffitt Cancer Center, and Maen Hussein, MD, of Florida Cancer Specialists and Research Institute.
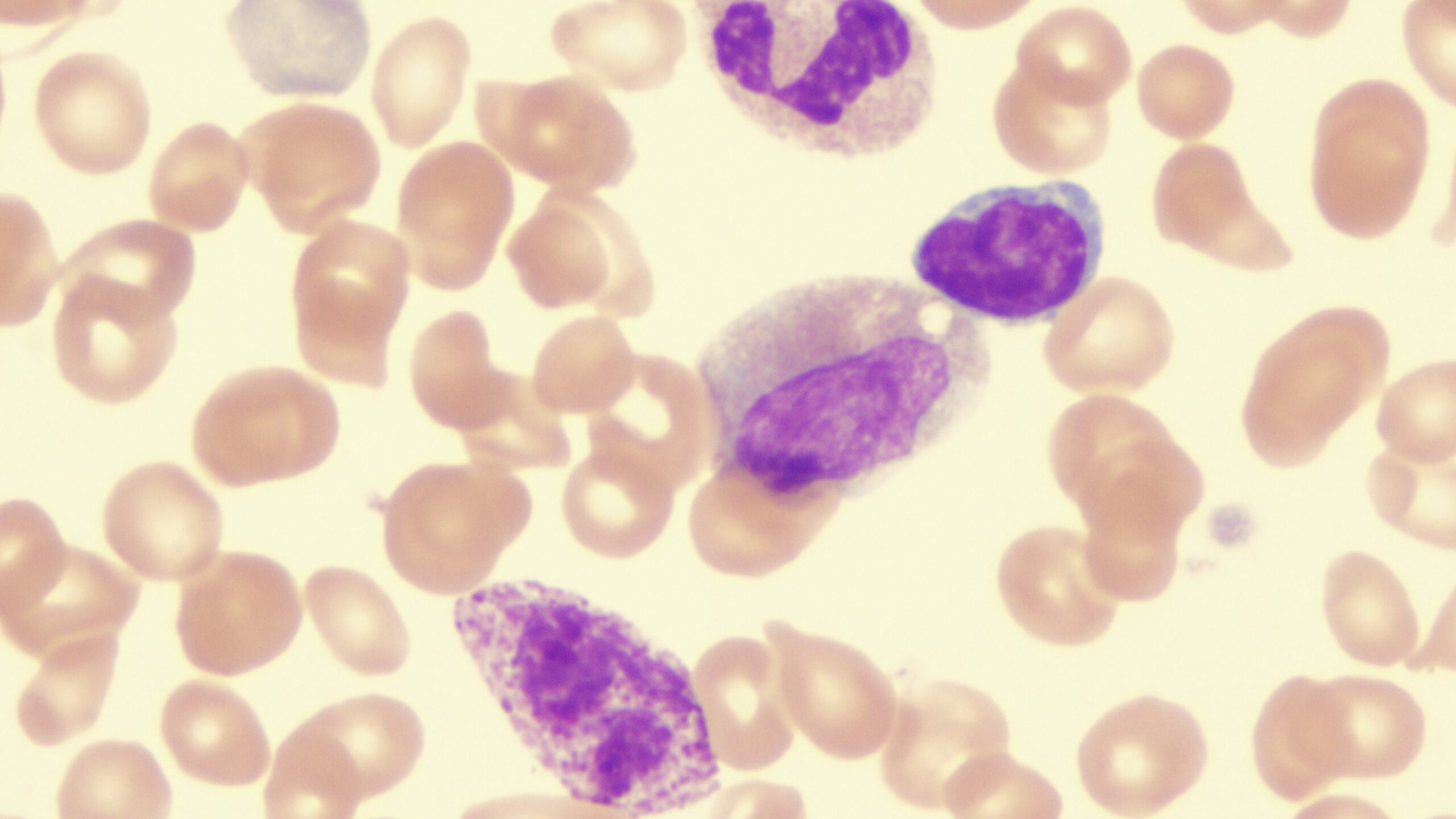
Avapritinib Among Tyrosine Kinase Inhibitors for Systemic Mastocytosis
In his presentation on systemic mastocytosis, Dr. Bose highlighted that the majority of patients have KIT mutations—the most common of which is KIT D816V—and several targeted therapies are available now. As he compared avapritinib, bezuclastinib, and elenestinib, he especially focused on avapritinib, which targets KIT D816V. In both the EXPLORER and PATHFINDER trials, this agent resulted in an impressive overall response rate of 75%, with the EXPLORER cohorts having better survival than has been seen historically.1
However, the larger panel engaged in a heavy discussion of avapritinib’s side effects. Dr. Kuykendall pointed out that although the agent is effective, it is not recommended for patients with platelet counts lower than 50,000 due to risk of intracranial hemorrhage.
“I think there are KIT inhibitors that could match it in efficacy without side effect issues,” Dr. Kuykendall said.
Dr. Bose concurred with this platelet count recommendation to avoid intracranial bleeding and also cited avapritinib’s cognitive side effects. He noted that the approved dose of 25 mg, given orally once daily for this drug, has almost no toxicity but he stops use immediately if he sees any in a patient. Avapritinib also differs from both bezuclastinib and elenestinib in that it penetrates the blood-brain barrier. This observation launched a discussion about such penetration and the risk of brain fog.
“Drug nonpenetration of the blood-brain barrier is considered a good thing, but the disease can penetrate the blood-brain barrier, too, so we wonder if [we] need the drug to penetrate too to treat it. The disease itself, too, can cause brain fog,” Dr. Bose said.
Ruxolitinib Among JAK Inhibitors for Myelofibrosis
Dr. Kuykendall’s presentation on myelofibrosis treatments focused on 4 Janus kinase (JAK) inhibitors: ruxolitinib, fedratinib, pacritinib, and momelotinib.2
One of the 3 newer agents, fedratinib, has demonstrated the best spleen volume reduction of all 4 and has shown encouraging second-line data in the JAKARTA-2 and FREEDOM-2 studies. Pacritinib was very recently discovered to be a potent activin A receptor, type 1 (ACVR1) inhibitor and to provide anemia benefit favorable over best available therapy. Regarding momelotinib, the results of the SIMPLIFY-1 and SIMPLIFY-2 trials led to the phase 3 MOMENTUM study in which momelotinib was found to be superior to danazol overall, including in anemia care.2
“Momelotinib was better at spleen response, but we want to use it most in patients with anemia, and here we saw encouraging results.” Dr. Kuykendall said.
Regarding ruxolitinib, the experts on the panel commonly spoke of the symptom relief their patients experience, often within days of starting it. Dr. Hussein said that the most common feedback from his patients about this drug is, “I feel better,” even if biomarkers did not improve or the spleen did not shrink. Dr. Bose has observed the same and mentioned that he prescribes ruxolitinib earlier for patients more frequently.
“More data is showing up saying it can be disease modifying if you go in early,” Dr. Bose clarified.
Dr. Kuykendall is also prescribing the drug earlier but finds response varies by symptoms present; for example, it is less impressive if patients have just fatigue rather than both fatigue and night sweats. Moreover, the different mutations that can feature in the disease affect efficacy.
“We don’t see across-the-board improvement with the disease. Long-term benefit is seen usually in those with just one mutation,” Dr. Kuykendall clarified.
Dr. Hussein mentioned a 79-year-old patient in a clinical trial who has improved after nearly a year of treatment with ruxolitinib, which raised the question of how to confirm whether benefit is due to ruxolitinib or a combination treatment. Dr. Kuykendall said it is still unclear how to design clinical trials to answer this question, although he suspects disease control ultimately requires combination therapy.
“We don’t know what the proper end points for control should be for these trials, such as spleen size reduction. Does it matter to shrink the spleen a little bit more?” Dr. Kuykendall elaborated.
References
- Bose P. Systemic mastocytosis. Presented at: The Fourth Annual National General Medical Oncology Summit; February 28 to March 3, 2025; Miami, Florida.
- Kuykendall A. State of the art treatment of myelofibrosis. Presented at: The Fourth Annual National General Medical Oncology Summit; February 28 to March 3, 2025; Miami, Florida.


 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.