Results from a new observational study presented at Transcatheter Cardiovascular Therapeutics (TCT) 2020 showed that untreated lesions with abnormal fractional flow reserve (FFR) but intact coronary flow reserve (CFR) do not have non-inferior outcomes compared to untreated lesions with normal FFR.
Observational data has previously suggested that lesions with intact CFR (CFR≥2) do well, though few studies have simultaneously assessed FFR, which has become a reference standard for guiding decisions for revascularization. DEFINE-FLOW was designed to assess whether vessels with abnormal FFR (FFR≤ 0.8) and intact CFR will achieve non-inferior outcomes compared to lesions with FFR>0.8 and CFR≥2 when treated medically. The primary endpoint was composite all-cause death, myocardial infarction, and revascularization at two years.
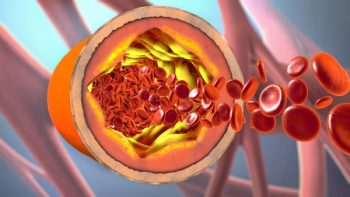
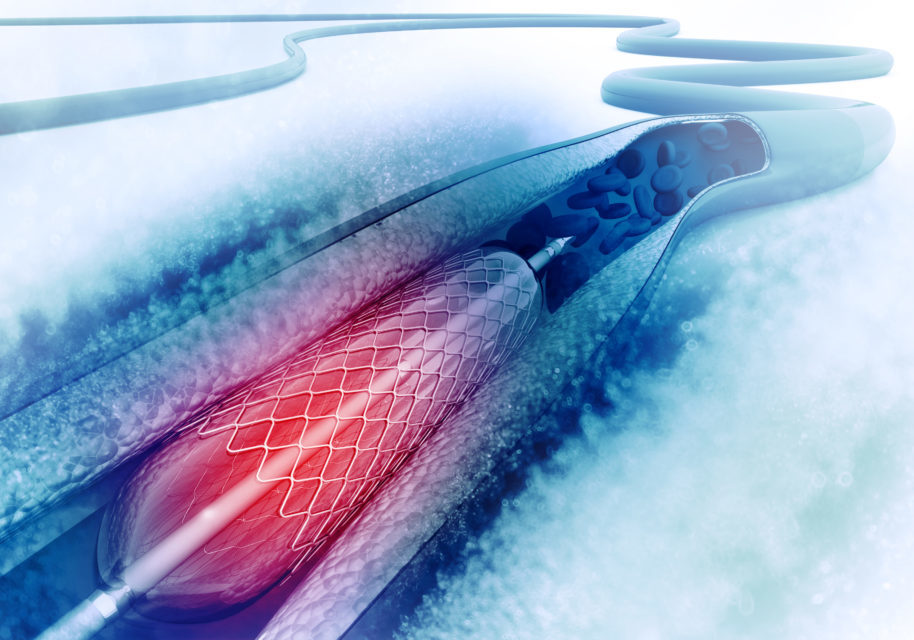
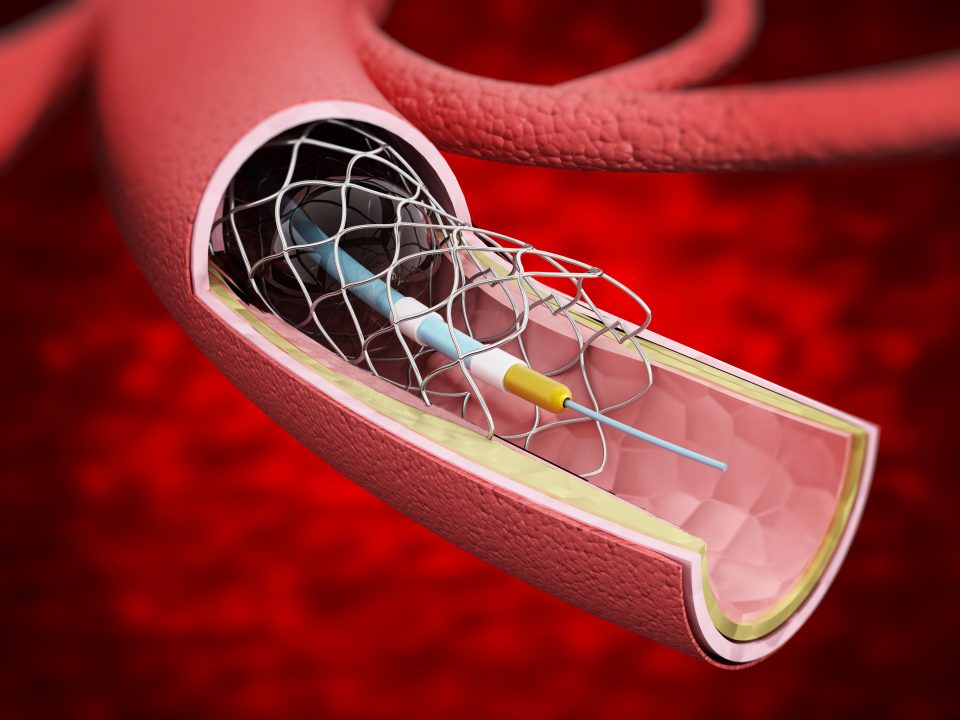
Stable coronary lesions from 430 patients underwent simultaneous FFR and CFR assessment with central core lab review of the tracings. Lesions with both FFR≤0.8 and CFR<2.0 underwent percutaneous coronary intervention (PCI), while for all other combinations, including FFR≤0.8 but intact CFR>2.0, PCI was deferred, and initial medical therapy was delivered. Follow-up continued for two years.
Rates of Major Adverse Cardiovascular Events (MACE) at two years were 5.8% for FFR-/CFR-, 10.8% for FFR+/CFR-, 12.4% for FFR-/CFR+, and 14.4% for FFR+/CFR+ (after PCI). There was a 5.0% difference in rates for FFR+/CFR- compared to FFR-/CFR- (95%CI, -1.5% to +11.5%, p-value=0.065 for non-inferiority). The predetermined margin for non-inferiority was <10.0%, therefore vessels with abnormal FFR≤0.8 but intact CFR≥2.0 did not show non-inferior outcomes compared to those with normal FFR.
“Because the study was observational, it is not clear what the outcomes among FFR+/CFR-lesions would have been had they undergone PCI instead of medical therapy,” Nils Johnson, MD, McGovern Medical School at UTHealth, and study co-author, commented in a press release. “There were a number of limitations to this study such as few lesions with severe FFR/CFR as well as unblinded subjects and physicians. The limitations coupled with the results makes this a hypothesis-generating study that can help to further understand the role of invasive CFR and how to treat CFR/FFR discordance.”
Nils J. The DEFINE-FLOW Study: Combined CFR and FFR Assessment. Presented at TCT 2020.



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.