Heart failure (HF) incidence, prevalence, and management is associated with the socioeconomic status of individuals and their communities, according to research from the American College of Cardiology Annual Scientific Session.
“HF outcomes are a complex interplay of clinical factors, individual socioeconomic status, neighborhood effect, and quality of care provided,” said Sameed Ahmed M. Khatana, MD, of the University of Pennsylvania, who discussed HF in vulnerable populations during a session titled, “Health Care Policy in HF: Implications for Vulnerable Populations.” He talked about two policy programs that attempt to incentivize quality of care and can help more vulnerable populations.
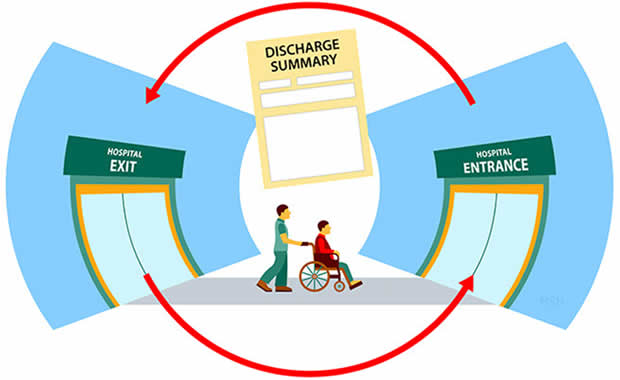
The Hospital Readmission Reduction Program (HRRP) seeks to reduced Medicare inpatient payments to hospitals for “excess” readmissions. It penalizes access readmission based on the following ratio: predicted to expected hospital readmission based on an average hospital with similar case-mix index. However, HRRP may disproportionately impact hospitals where patients of lower socioeconomic status receive care. Safety-net hospitals (SNHs) provide a disproportionate share of uncompensated care and have a higher likelihood of being penalized.
In fiscal year (FY) 2018, HRRP fined 2,573 hospitals (around 80% of all hospitals evaluated). In FY 2017, SNHs received an average penalty of 0.70% compared with 0.51% for the hospitals in the lowest quartile.
“This might not seem [like] much; however, for many hospitals that are already financially constrained, this is a significant financial burden,” said Dr. Khatana. “According to one estimate, for rural SNHs, more than 40% already operate with a negative profit margin.”
While no single approach has been demonstrated to consistently reduce readmission rates, a multipronged approach appears to be helpful. However, SNHs report more barriers to implementing strategies, as well as lower utilization. SNHs are less likely to track readmissions, incentivize leadership and providers to reduce readmissions, use health information technology tools, use dedicated staff members/resources targeted at discharges and readmissions, and use post-discharge strategies/programs, according to a 2017 study published in Medical Care.
There are some upcoming changes that may address this problem with HRRP. The 21st Century Cures Act requires the Centers for Medicare & Medicaid Services (CMS) to account for socioeconomic status when comparing hospitals in HRRP. Starting in FY 2019, CMS will only compare hospitals in the same quintile based on proportion of dual-eligible beneficiaries. This is expected to reduce penalties for SNHs, potentially up to an average of 25%, but it will lead to increased penalties for non-SNHs, as the mandate requires a program to be overall budget-neutral compared with previous years, according to Dr. Khatana.
The Hospital Value Based Purchasing Program (VBP) adjusts inpatient payments based on performance of several measures, including 30-day HF mortality. In FY 2020, CMS can withhold 2% of diagnosis-related group payments to provide $1.7 billion for program incentives. “Like HRRP, there is concern [for] how this will impact SNHs,” he said. There are small to no significant differences in 30-day HF mortality rates between SNHs and non-SNHs, but SNHs are still more likely to be penalized under VBP.
Accounting for patient socioeconomic status may “send a signal that people of lower socioeconomic status should be getting a lower standard of care,” Dr. Khatana cautioned.
He concluded the presentation by offering some potential solutions:
- Measuring and identifying causes of disparities
- Some measures may be more reasonable to adjust for socioeconomic than others
- Accounting for financial health of SNHs
- Identifying causes for heterogeneity among SNHs
- Payment models to incentivize care for vulnerable populations






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.