
The combination of eltrombopag and lenalidomide is effective and safe at treating certain patients with myelodysplastic syndrome (MDS), according to a study presented at the 2021 American Society of Hematology Annual Meeting. Jesus D. Gonzalez-Lugo, MD, and colleagues, presented the findings of this study.
As the researchers explained, lenalidomide is a Food and Drug Administration–approved therapy for the treatment of patients with MDS with del5q which has been shown to induce disease remission and transfusion independence in almost 65% of this population. For patients with MDS without del5q, lenalidomide appears to reduce transfusion needs in one-quarter of the population, but its use is limited by the risk of significant thrombocytopenia. Furthermore, patients with platelet counts <50×109/L have traditionally been excluded from clinical trials.
Eltrombopag is a thrombopoietin receptor agonist (TPO-RA) that has proven to be effective in increasing platelet counts in patients with MDS. Preclinical data also has demonstrated that eltrombopag can reverse the anti-megakaryopoietic effects of lenalidomide in MDS patient samples.
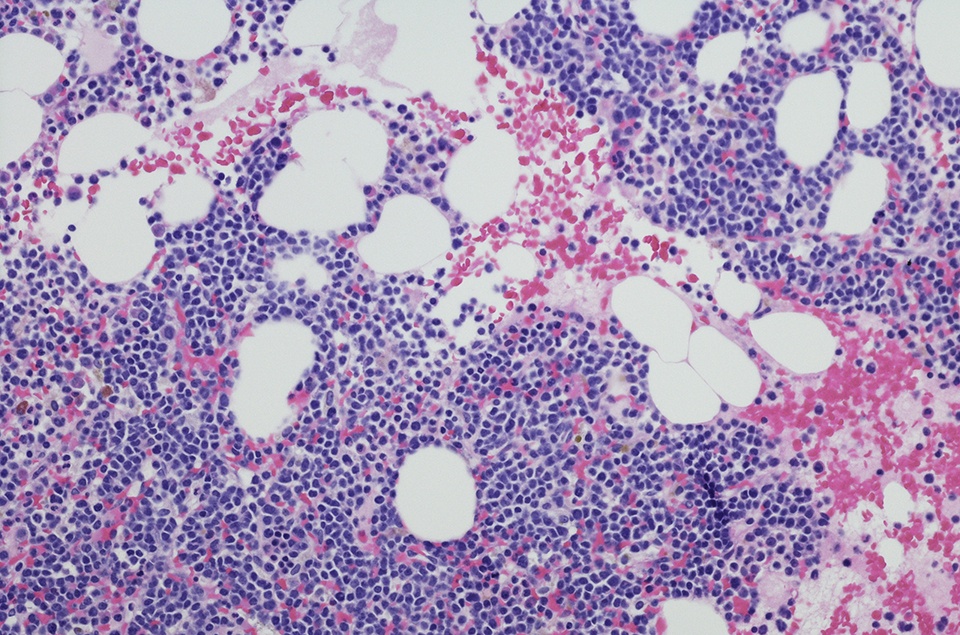
The present study was designed to evaluate the safety and efficacy of the combination of eltrombopag and lenalidomide in patients with low- and intermediate-risk MDS (per International Prognostic Scoring System-Revised; IPSS-R) or non-proliferative chronic myelomonocytic leukemia (CMML). Researchers enrolled 44 patients aged 18 years and older with symptomatic anemia and without prior exposure to either lenalidomide or eltrombopag.
Of the 44 evaluable participants (out of 51 enrolled), most were male (70%), median age was 71 years, and 95% of patients had MDS and 5% had CMML More than half of patients (n = 24; 55%) had low-risk MDS per IPSS-R score. Two-thirds were treatment-naïve and 16 patients (36%) had received one or more lines of treatment, including erythropoiesis-stimulating agents.
Patients were treated according to platelet counts at baseline: Arm A included patients with platelet counts ≥50×109/L who received lenalidomide alone at 10 mg daily on days 1 through 21 of each 28-day treatment cycle. If platelet counts fell below 50×109/L, lenalidomide was discontinued and eltrombopag was administered on days 1 through 28 until platelet levels exceeded 50×109/L for two weeks; at that point, patients resumed lenalidomide. If platelet counts dropped below 50×109/L again, patients received eltrombopag on the same schedule, along with concomitant lenalidomide. In Arm B, patients with platelet counts <50×109/L received eltrombopag on days 1 through 28 until platelet counts reached ≥50×109/L, then the same treatment as patients in Arm A.
The eltrombopag-lenalidomide combination was well-tolerated, the authors reported, with few non-hematologic grade 3-4 treatment-related adverse events (AEs). These AEs included grade 3 hyperbilirubinemia (7%), grade 3 transaminitis (2%), grade 3 diarrhea (2%), and grade 3 arthralgias (2%). Two patients had major bleeding events and two patients died (attributable to pneumonia and gallbladder cancer). Of the 31 patients who received eltrombopag, one had a reversible increase in peripheral blasts while on treatment, and one patient developed marrow fibrosis after six years on treatment.
In terms of efficacy, the objective response rate (ORR) in the intent-to-treat population (n = 51) was 35% (32% in arm A and 39% in arm B). A total of 13 (30%) patients achieved red blood cell transfusion-independence (RBC-TI).
Of the 17 patients who received eltrombopag alone, the ORR was 41% (n = 7/17), with 29% achieving bilineage responses. For comparison, of the 13 patients who received lenalidomide alone, ORR was 46% (n = 6/13), all of whom achieved RBC-TI. When looking at the eltrombopag-lenalidomide combination, the ORR was 36%, two patients achieved bilineage responses, and two achieved complete response.
“Treatment with eltrombopag-lenalidomide demonstrates good efficacy with an ORR of 40.9%, response durability, and an acceptable safety profile for evaluable patients with low-/intermediate-risk MDS,” the researchers concluded. “Eltrombopag can lead to single-agent responses with an acceptable safety profile and sizable proportion of multilineage responses.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.