
Chimeric antigen receptor (CAR) T-cell therapy is a potentially life-saving option for patients with hematologic cancers, but it may lead to higher use of healthcare resource utilization after infusion, according to an analysis of real-world data presented at the 2021 American Society of Hematology Annual Meeting.
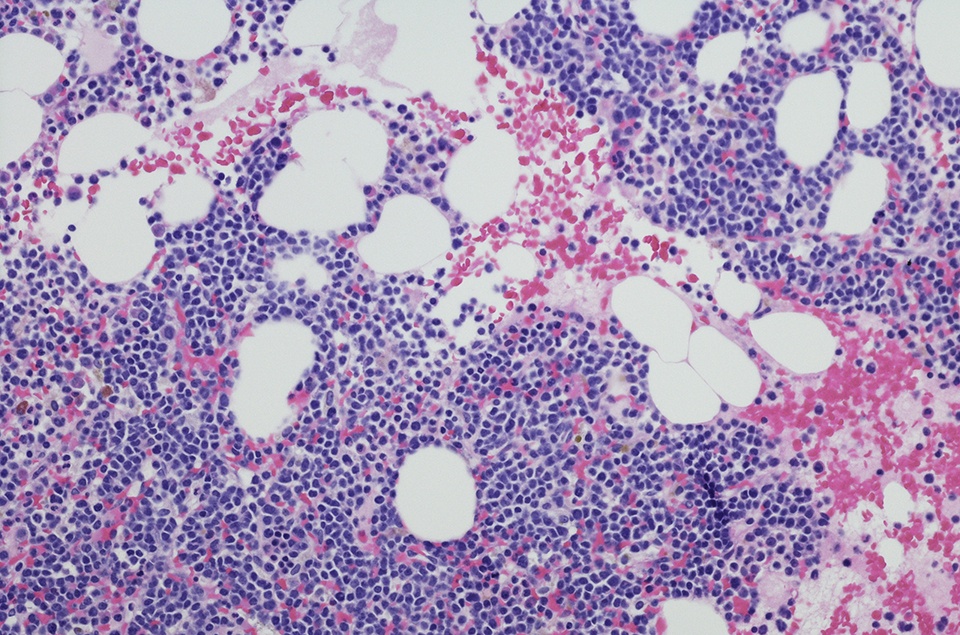
Researchers examined hospitalizations and emergency department (ED) visits for the first 12 months subsequent to CAR T-cell infusion to better understand health-care resource use among these patients. They used the Truven Health MarketScan database to identify commercially insured patients under the age of 65 who received CAR T-cell infusion between January 2017 and December 2019. CAR T-cell therapy administration was discerned using ICD-10 codes as well as national drug codes for axicabtagene ciloleucel and tisagenlecleucel. Patients of interest were followed for hospitalizations and/or ED visits from CAR T-cell infusion to death, and loss of coverage at 12 months or the conclusion of the study period, whichever came first. Patient diagnoses included chronic lymphocytic leukemia (CLL), diffuse large B-cell lymphoma (DLBCL), and multiple myeloma.
Overall, the study assessed 204 patients (66% male) who received CAR T-cell infusions (96% tisagenlecleucel) over the three-year analysis period.
With respect to hospitalizations, the results showed that 44% of patients had 191 hospitalizations within 12 months of CAR T-cell infusion. The investigators observed that 16% of all CLL patients, 12% of all DLBCL patients, and 11% of all myeloma patients had more than two hospitalizations. The most prevalent reasons for hospitalization were infection (41.3% of hospitalizations), myelosuppression (19.9%), and management of underlying malignancy (18.3%). Patients hospitalized for infection had the longest duration of stay per hospitalization (13.5 days), followed by management of underlying malignancy (8.3 days), and myelosuppression (5.9 days).
In terms of ED visits, the findings showed that a quarter of patients (25%) had 71 ED visits following CAR T-cell infusion. Reasons for ED visits included infections (19.7%), myelosuppression (15.5%), and cardiac emergencies (8.5%).
“The probability of these hospitalizations is highest within the first month, declining rapidly thereafter,” the researchers concluded. They added that these findings “can be used to inform management strategies to mitigate unplanned healthcare utilization.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.