First-line treatment with the autologous anti-CD19 chimeric antigen receptor (CAR) T-cell therapy axicabtagene ciloleucel (axi-cel) led to rapid responses in patients with high-risk large B-cell lymphoma (LBCL), according to results from the phase II ZUMA-12 trial. These data were presented at the 2021 American Society of Hematology Annual Meeting by Sattva S. Neelapu, MD.
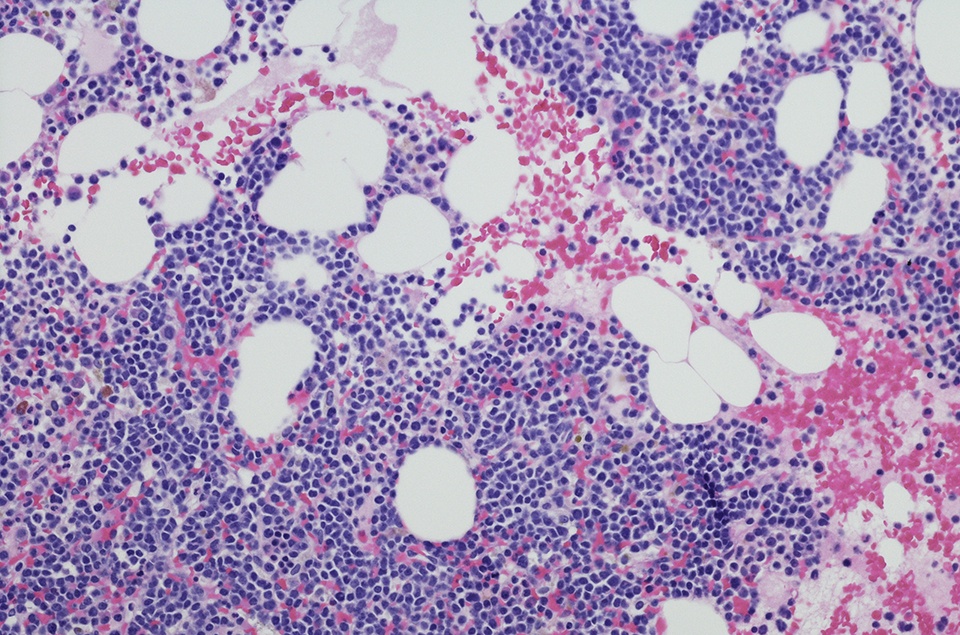
As of data cut-off, the multicenter, single-arm ZUMA-12 study had enrolled 42 patients with high-risk LBCL, 40 of whom had received axi-cel at the time of the data presentation.
Prior to CAR T-cell infusion, patients underwent leukapheresis and conditioning chemotherapy with cyclophosphamide and fludarabine. Axi-cel was infused at 2×106 CAR T cells/kg. The primary endpoint was complete response (CR) rate, and secondary endpoints were objective response rate (ORR), duration of response (DOR), event-free survival (EFS), progression-free survival (PFS), overall survival (OS), adverse events (AEs), and levels of CAR T cells and cytokines. All patients had follow-up of at least six months.
Participants’ median age was 61 years (range = 23-86 years). Sixty-eight percent of the cohort was male, and most patients (95%) had stage III/IV disease. Thirty-seven patients were evaluable at data cut-off, with a median of 15.9 months of follow-up (range = 6.0-26.7). Most patients (89%) at least partially responded to treatment, and median time to response was one-month post-infusion. Twenty-nine patients (78%) achieved a CR. At cut-off, 73% of patients had an ongoing response. Although medians for DOR, EFS, and PFS were not reached, the 12-month estimates for each of these measures were 81%, 73%, and 75%, respectively. Estimated 12-month OS was 91%. CAR T-cell levels in blood peaked at a median of eight days post-infusion (range = 8-37).
Among all 40 treated patients, the ORR was 90% at cut-off, with an 80% CR rate. In the overall treated population, all 40 patients experienced AEs, and 85% had grade ≥3 AEs. The most common grade ≥3 AE was cytopenia, occurring in 68%. Three patients (8%) experienced grade ≥3 cytokine release syndrome (CRS) and nine patients (23%) experienced neurologic events, with median onset times of four days and nine days, respectively. All cases of CRS resolved by the data cut-off, as did all but one case of neurologic event.
“With 15.9 months of median follow-up, responses were durable as medians for DOR, EFS, and PFS were not yet reached and over 70% of patients remained in response at data cut-off,” the authors summarized. “No new safety signals were reported with axi-cel in an earlier line. Overall, axi-cel may benefit patients exposed to fewer prior therapies, and further trials in first-line high-risk LBCL are warranted to assess axi-cel in this setting,” they concluded.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.