Akhila Vadivelan, MD, Discusses Iron Deposition in Transfusion-Dependent SCD
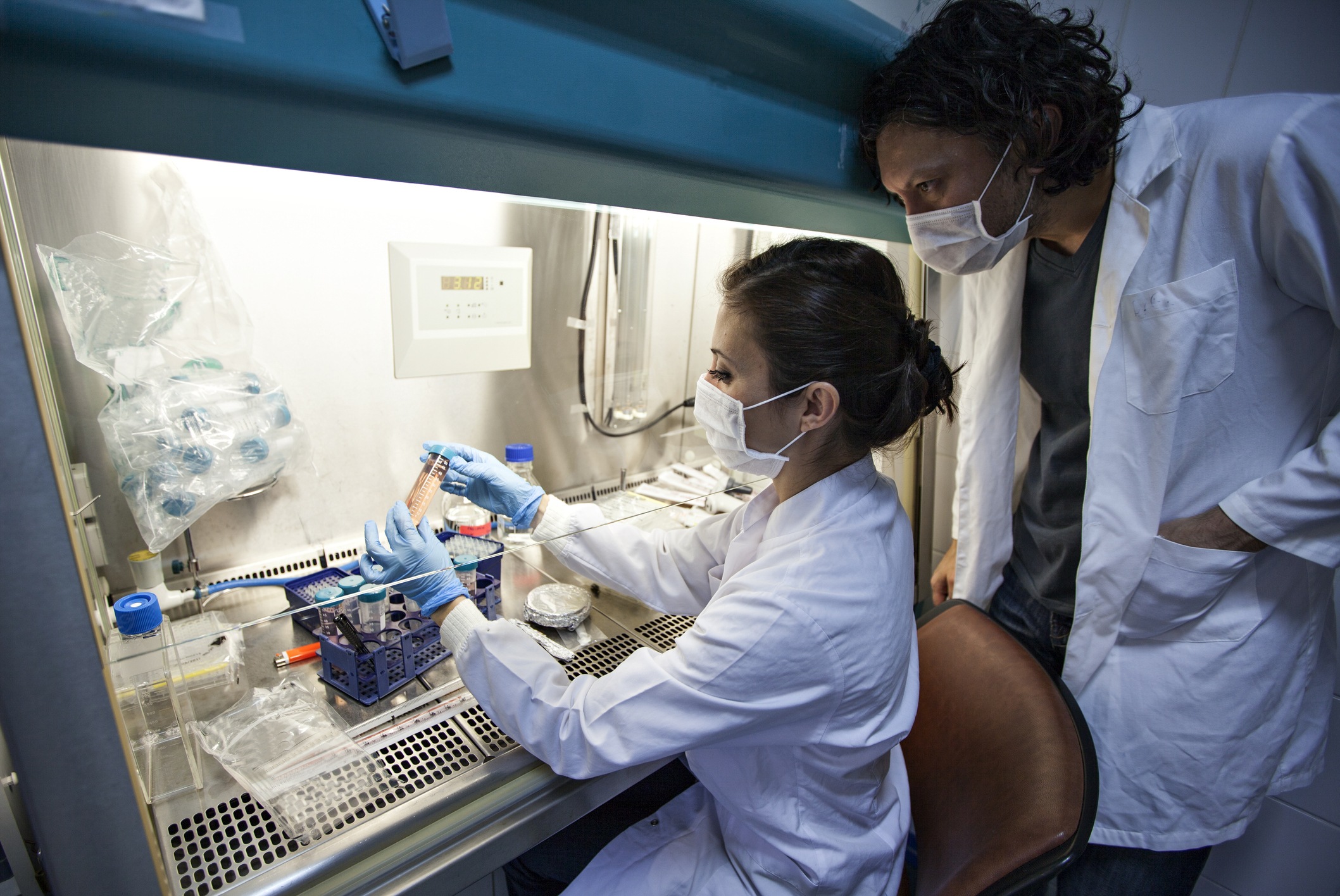
By Patrick Daly - Last Updated: April 23, 2024Dr. Vadivelan, of the UCLA Mattel Children’s Hospital, shared her study on pituitary and pancreatic iron deposition in patients with sickle cell disease (SCD) dependent on transfusions. She presented the findings at the 2024 American Society of Pediatric Hematology/Oncology Conference.
“Most hemoglobinopathies, such as SCD and thalassemia, are dependent on blood transfusions,” Dr. Vadivelan said. “With each milliliter of blood, 0.8 milligrams of iron goes into the body. The problem is there’s no way to excrete the excess iron. What happens to the excess after the bone marrow takes up all the iron for making new blood cells?”
She explained that excess iron is deposited into various other organs, including the pancreas, pituitaries, and heart. Pituitary iron deposition can lead to pituitary and gonadal dysfunction, pancreatic iron deposition can lead to diabetes, and iron deposition in the heart can lead to heart failure.
Dr. Vadivelan also noted that magnetic resonance imaging (MRI) replaced liver biopsy as standard-of-care for detecting how much iron is present in a patient.
“This study focused on trying to determine the prevalence, predictors, and significance of pituitary iron in chronically transfused SCD patients,” Dr. Vadivelan said. “We did a cross-sectional analysis of all patients with SCD who had undergone a brain MRI between 2009 and 2022 and had MRIs with pituitary volume and iron.”
“Surprisingly, we found that 73% of patients had pituitary iron, and about 27% of them were in the range that is associated with hypogonadism in patients with thalassemia,” she continued.
According to the study, the best overall predictors for severe pituitary iron deposition were liver iron concentration and ferritin; however, the best multivariate predictor was ferritin plus years of transfusion therapy. Additionally, Dr, Vadivelan and colleagues reported that higher pituitary iron was associated with reduced pituitary volume.
“This study is really remarkable in the sense that we were able to figure out that patients were younger and had pituitary iron even before pancreatic iron, which was not found before,” Dr. Vadivelan summarized. “None of our patients had a clinical diagnosis of hypogonadism.”
She concluded with the suggestion that all physicians “keep a high index of suspicion for iron overload-mediated hypogonadism in chronically transfused SCD patients.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.