
Researchers have recently used an artificial intelligence (AI) system to accurately predict side effects associated with radiation therapy for head and neck cancer. This precise computer model has the potential to prevent excessive weight loss after cancer treatment and decrease the need for a feeding tube. This work was presented at the 61st Annual Meeting of the American Society for Radiation Oncology (ASTRO).
“In the past, it has been hard to predict which patients might experience these side effects,” explained lead author Jay Reddy, MD, PhD, an assistant professor of radiation oncology at The University of Texas MD Anderson Cancer Center. “Now we have a reliable machine learning model, using a high volume of internal institutional data, that allows us to do so.”
Head and Neck Cancer
Roughly 53,000 patients diagnosed with head and neck cancers in the US each year. Men are more than twice as likely to receive this diagnosis as women, with the average age at diagnosis being 62 years. When detected early in the disease progression, head and neck cancers are usually treated with surgery or radiation therapy. A combination of radiation and chemotherapy is typically administered to patients with more advanced disease.
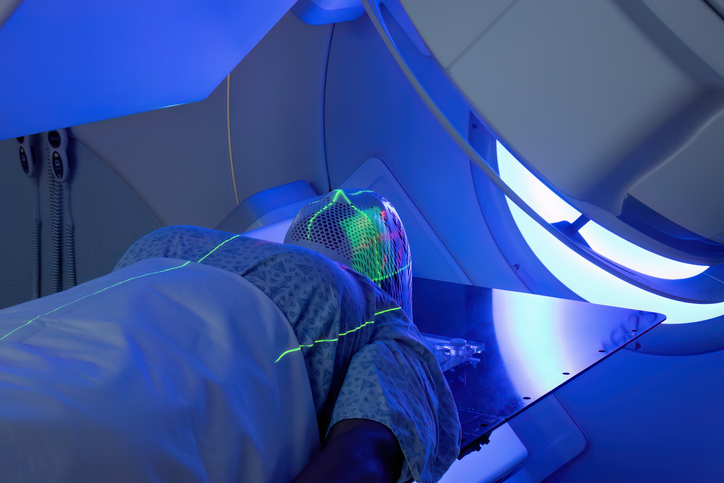
Although radiation is effective in combatting the growth of new cancer cells, it also manifests damage to oral tissue and can alter the mouth’s bacterial composition, leading to sore throat, loss of taste, and other adverse effects. If the soreness is too severe for the patient to eat, this can cause weight loss and the need for feeding tube insertion.
“Being able to identify which patients are at greatest risk would allow radiation oncologists to take steps to prevent or mitigate these possible side effects,” said Reddy. “If the patient has an intermediate risk, and they might get through treatment without needing a feeding tube, we could take precautions such as setting them up with a nutritionist and providing them with nutritional supplements. If we know their risk for feeding tube placement is extremely high – a better than 50% chance they would need one – we could place it ahead of time so they wouldn’t have to be admitted to the hospital after treatment. We’d know to keep a closer eye on that patient.”
A Machine Learning Solution
Reddy and colleagues created machine learning models to analyze data from electronic health records (Epic), an internal web-based charting tool (Brocade), and the record/verify system (Mosaiq). This data consisted of over 700 clinical and treatment variables for head and neck cancer patients. The average age in this patient population was 62 years and 75% of these patients were male. Each of these subjects had received over 2,000 courses of radiation therapy across five different practice sites at MD Anderson between 2016 and 2018.
Significant weight loss, feeding tube placement, and unplanned hospitalizations were the three endpoints that the AI models were used to predict in these patients. The results from the most accurate model were then validated using data from 225 consecutive radiation therapy treatments. Machine learning models with a performance rate that achieved the defined area under the curve (AUC) threshold of 0.70 (indicating 70% accuracy) were deemed clinically acceptable.
The researchers found that their machine learning models predicted the likelihood of significant weight loss and need for feeding tube placement with AUC’s of 0.751 and 0.755, respectively, indicating high accuracy.
“The models used in this study were consistently good at predicting those two outcomes,” said Dr. Reddy. “You could rerun those models with a new patient or series of patients and get a number saying this adverse effect is likely to happen or not to happen.”
He explained that using this model, the physician can input patient-specific data such as age, gender, and cancer type, and see what their potential risk would be for needing a feeding tube or experiencing severe weight loss.
Despite this success, the AI was unable to accurately predict the unplanned hospitalizations with appropriate accuracy, yielding an AUC of only 0.64. Reddy and colleagues believe that redoing their analyses with more data could improve the model’s ability to predict this outcome.
“As we treat more and more patients, the sample size gets bigger, so every data point should get better,” he said. “It’s possible we just didn’t have enough information accumulated for this aspect of the model.”
Although this AI system cannot identify the single-most predictive factor/combination of factors that generate these negative outcomes, it can provide the patient and physician with a better idea of what to expect. Reddy added that machine learning models also have the potential to predict which treatment plans best suit each patient as well.
“Machine learning can make doctors more efficient and treatment safer by reducing the risk of error,” said Dr. Reddy. “It has the potential for influencing all aspects of radiation oncology today – anything where a computer can look at data and recognize a pattern.”
At the ASTRO Annual Meeting, researchers unveil the latest research in areas such as cardiac radioablation, immunotherapy and machine learning https://t.co/gqMKyU0pG7
— Angel Montero Luis (@Monthy_A) September 20, 2019





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.