Certain patients with psoriasis who receive the Johnson & Johnson COVID-19 vaccine may want to temporarily stop taking their medication, according to guidance from the National Psoriasis Foundation (NPF).
Specifically, patients aged ≥60 years with at least one comorbidity linked to poorer COVID-19 outcomes who have well-controlled disease on methotrexate “may, in consultation with their prescriber, consider holding it for 2 weeks” following vaccination, the recommendation states.
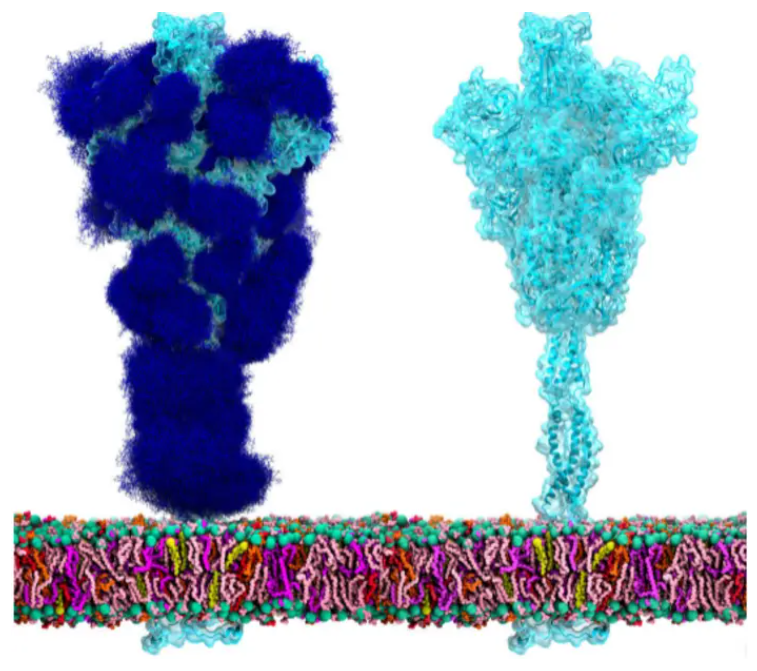
The guideline is one of 29 recommendations suggested by the NPF COVID-19 Task Force and pertains specifically to the “replication-incompetent adenovirus type 26-vectored vaccine encoding a stabilized variant of the SARS-CoV-2 S protein (Ad26.COV2.S, manufactured by Johnson & Johnson),” the Task Force clarifies.
The reason it may be recommended to temporarily stop taking methotrexate is based on information known about the flu shot: when receiving a flu vaccination, patients with rheumatoid arthritis who took a two-week break from methotrexate after their shot showed “a modest improvement in antibody titer response, with unknown clinical significance.” Whether this will be the case for the COVID-19 vaccines remains unknown, which is why the Task Force recommends patients discuss their treatment plan with their provider. “Shared decision-making between clinician and patient is recommended to guide discussions about use of systemic therapies during the pandemic,” according to the guidance.
The one-shot Johnson & Johnson vaccine is different from the Moderna and Pfizer vaccines, which are mRNA-based and are currently given in two doses. The Task Force recommends that patients with psoriasis receive either the Pfizer or Moderna vaccine, but if given the choice between the Johnson & Johnson shot or not being vaccinated at all, it’s best to take the vaccine that’s available.
Patients who receive one of the mRNA-based vaccines may not have to pause biologic or oral therapies, but they should have a conversation with their provider. The Task Force also notes, “Systemic medications for psoriasis or psoriatic arthritis are not a contraindication to any currently available COVID-19 vaccines.”
A study that came out earlier this year found that while about half of patients with autoimmune diseases are willing to get the COVID-19 vaccine, about a third remain uncertain about it, suggesting there is an opportunity for healthcare professionals to provide education to their patients.
“Importantly, the willingness to get vaccinated against SARS-CoV-2 increased when vaccination was recommended by a physician, and the most trusted health-care professionals was the specialist physician. These data show the crucial and timely role of rheumatologists in vaccination uptake,” the study authors observed.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.