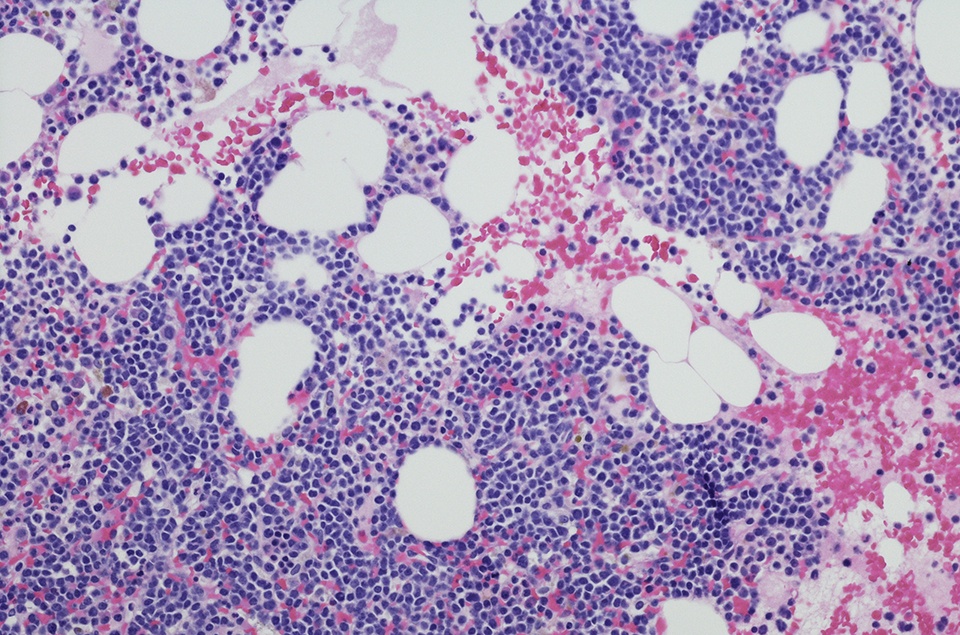
In an open-label, multicenter study presented at the 2021 ASH Annual Meeting, the combination of sabatolimab and hypomethylating agents (HMAs) was well-tolerated and led to durable clinical responses in patients with very high/high-risk myelodysplastic syndrome (vHR/HR-MDS) and newly diagnosed acute myeloid leukemia (AML). The results represented updated data from a phase Ib study, which included 53 patients with vHR/HR-MDS and 48 patients with newly diagnosed AML.
Sabatolimab is an immunotherapeutic therapy targeting TIM-3 on immune and myeloid cells. Study investigators evaluated the safety and tolerability of sabatolimab plus HMAs. Other objectives were assessment of preliminary efficacy, via overall response rate (ORR), duration of response (DOR), and progression-free survival (PFS). The investigators evaluated the proportion of patients who experienced a possible immune-mediated adverse event (imAE) in patients who achieved disease remission.
The most common grade ≥3 adverse events (AE), reported in 15% or more patients, included thrombocytopenia, neutropenia, anemia, and febrile neutropenia.
During the study, six patients with vHR/HR-MDS and 10 with ND-AML experienced possible imAEs. The researchers reported that few patients experienced clinically significant possible imAEs, and no grade ≥3 possible imAEs were reported in the vHR/HR-MDS group. Five patients with newly diagnosed AML experienced grade 3 imAEs, but none of the patients had grade 4/5 possible imAEs.
“The observed relationship between response and possible imAEs in vHR/HR-MDS would need further confirmation in ongoing studies, but suggests that an immunomodulatory mechanism of sabatolimab may be contributing to clinical responses,” the researchers wrote.
The authors also noted that nearly 25% of patients with vHR/HR-MDS experienced a degree of improvement that allowed them to undergo hematopoietic cell transplantation (HCT).
In the 51 patients with vHR/HR-MDS who were considered evaluable for response, the ORR was 56.9%. Additionally, the median DOR in the vHR/HR-MDS group was 16 months, while the median DOR in patients with CR was 21.5 months.
The estimated 12-month PFS was 51.9%. In the 40 patients with newly diagnosed AML, the ORR was 40.0% and the median DOR was 12.6 months. In addition, the median DOR in patients with CR was 23.0 months. The estimated 12-month PFS rate in the newly diagnosed AML population was 27.9%.
According to the investigators, there were durable responses in patients with adverse-risk mutations, including patients with vHR/HR-MDS and TP53 mutations (ORR = 71.4%; median DOR = 21.5 months) and patients with newly diagnosed AML and ≥1 European LeukemiaNet adverse-risk mutation (ORR = 53.8%; median DOR = 12.6 months).
The authors added that, in patients with vHR/HR-MDS who underwent HCT, outcomes were generally favorable following the transplant procedure in patients, and no excess toxicities related to graft-versus-host disease were reported.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.