
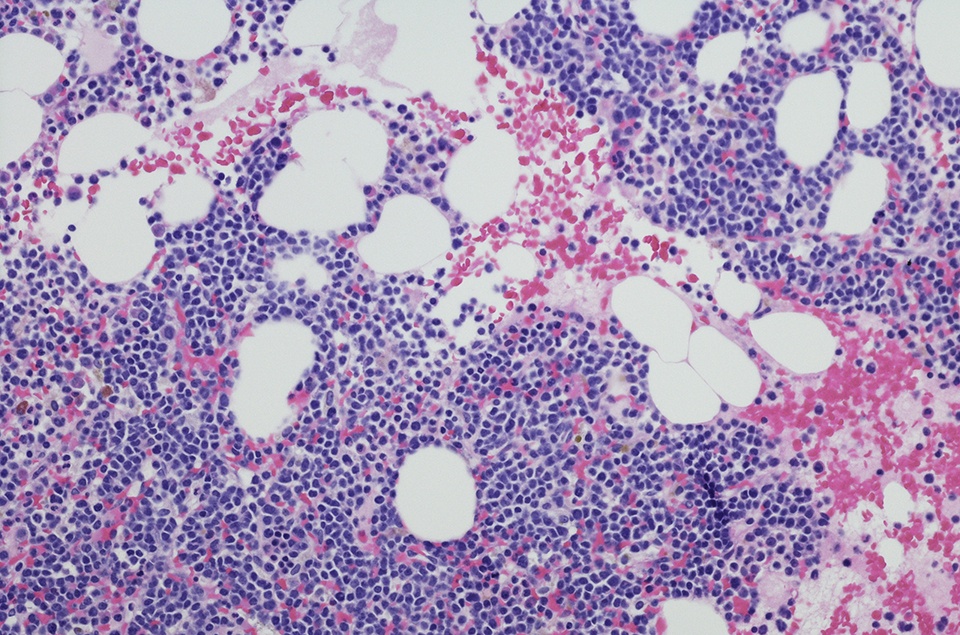
Acalabrutinib monotherapy demonstrated a sustained benefit for treatment of relapsed/refractory chronic lymphocytic leukemia (CLL) compared with standard-of-care regimens, according to three-year follow-up data from the ASCEND trial. These findings were presented at the 63rd American Society of Hematology (ASH) Annual Meeting & Exhibition.
In the primary analysis of the phase III randomized ASCEND study, at a median follow-up of 16.1 months, treatment with acalabrutinib led to prolonged progression-free survival (PFS) compared with idelalisib plus rituximab (ldR) or bendamustine plus rituximab (BR), with a favorable safety profile.
Patients were randomized 1:1 to either oral acalabrutinib 100 mg twice daily (n = 155) or investigators’ choice of eight cycles of IdR (n = 119) or six cycles of BR (n = 36). Treatment continued until disease progression or unacceptable toxicity. Patients who progressed on IdR or BR were allowed to crossover to acalabrutinib monotherapy.
At a median follow-up of 36.0 months for the acalabrutinib arm and 35.2 months for the IdR/BR arm, the overall response rates were 83% and 85%, respectively. Median PFS had not been reached in the acalabrutinib group, compared with 16.8 months in the IdR/BR arm (hazard ratio [HR] = 0.29, 95% confidence interval [CI] 0.21-0.41; p < 0.0001). The three-year PFS rates were 63% versus 21% in favor of acalabrutinib. The researchers noted that this PFS benefit was sustained regardless of IdR or BR treatment (all p < 0.0001).
Additionally, high-risk subgroups also experienced a PFS benefit with acalabrutinib treatment. Three-year PFS rates were 66% and 5% for acalabrutinib and IdR/BR, respectively, among patients with del17p mutations (HR = 0.13; p < 0.0001), and 61% and 17%, respectively, in patients with unmutated IGHV (HR = 0.3; p < 0.0001). Median OS was not reached in either treatment arm. The three-year OS rates were 80% for acalabrutinib and 73% for standard of care.
The most common adverse events (AEs) with acalabrutinib, occurring in ≥20% of patients, were headache, neutropenia, diarrhea, and upper respiratory tract infection. Similarlly, the most common AEs with IdR were diarrhea and neutropenia; for BR they were neutropenia, fatigue, infusion-related reaction, and nausea. Thirty-eight percent of acalabrutinib-treated patients reported serious AEs, compared with 63% of IdR patients and 26% of BR patients. The most common serious AEs were pneumonia (acalabrutinib 8%; IdR 9%; BR 3%), pyrexia (2%; 7%; 3%), and diarrhea (1%; 15%; 0%). AE-related discontinuation occurred in 21% of acalabrutinib-treated patients, compared with 65% and 17% for IdR- and BR-treated, respectively. The authors also noted the following events of clinical interest: all-grade atrial fibrillation/flutter (acalabrutinib, 6%; IdR/BR, 3%), all-grade hypertension (7%; 4%), all-grade major hemorrhage (3%; 3%), grade ≥3 infections (25%; 27%), and all-grade secondary malignancies (7%; 3%).
The authors noted that the tolerability profile of acalabrutinib in this study was in line with the primary analysis, and no new safety findings were identified with longer-term follow-up.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.