
Although individuals older than 80 years make up more than 20% of cases of chronic lymphocytic leukemia (CLL), this population is underrepresented in clinical drug trials, and data on treatment outcomes are limited. At the 63rd American Society of Hematology (ASH) Annual Meeting & Exhibition, researchers presented results from a pooled analysis of phase II and III studies of this patient population, hoping to expand the evidence base.
According to their findings, older patients with CLL experience favorable efficacy and survival outcomes with frontline targeted anti-leukemic treatments such as ibrutinib, idelalisib, and venetoclax.
The researchers pooled data from six studies conducted by the German CLL Study Group, comprising 716 total patients aged ≥80 years who received frontline treatment for CLL. The primary endpoints were overall survival (OS) and causes of death. Patients received at least one targeted agent as firstline therapy. Median follow-up was 51.8 months.
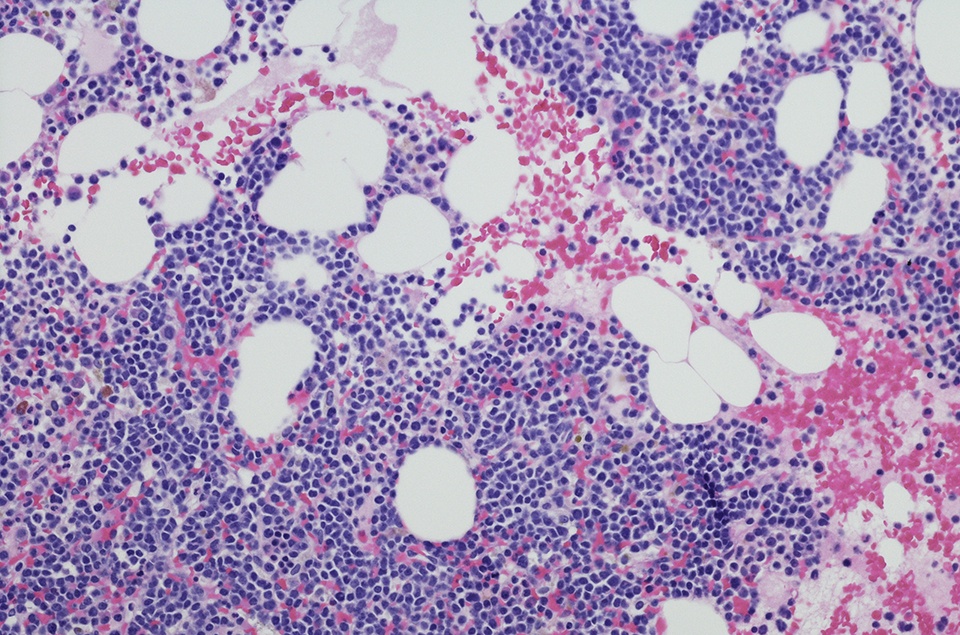
From the overall cohort, 33 patients (5%) were analyzed. The median age at treatment initiation was 82 years, and 55% of patients were male. Twenty-two patients (71%) had relevant comorbidities and 30 patients had impaired renal function. Sixty-nine percent of patients were categorized as high- or very-high risk. The most frequent frontline regimens were venetoclax plus obinutzumab (82%; n =27), bendamustine debunking with ibrutinib plus obinutuzumab (9%; n = 3), venetoclax plus obinutuzumab and ibrutinib (6%; n =2), and bendamustine with ibrutinib plus ofatumumab (3%; n = 1).
The overall response rate to treatment was 73%, with 36% of patients achieving a complete response. The rates of undetectable measurable residual disease in this subgroup were 73% in peripheral blood and 39% in bone marrow.
Three patients discontinued treatment due to progressive disease, four due to patient decision, and two due to “other” reasons. There were 11 fatalities overall, with five related to adverse events (AEs) and one each due to heart failure, pulmonary embolism, and renal failure. Other causes of death not related to AEs were progressive disease, infection, and respiratory insufficiency. One patient had an unknown cause of death. Nine secondary malignancies occurred in seven patients; the most common malignancy was basal cell carcinoma (44%).
According to time-to-event analyses, the median progression-free survival (PFS) was 49 months. The researchers reported that, in a matched cohort of patients younger than 80 years, median PFS was not yet reached. In the older patient cohort, the four-year OS rate was 68%, compared with 92% in the matched cohort. Median OS and median time-to-next-treatment were not reached.
Based on the average mortality rate in the ≥80 years age group, the standardized mortality ratio was 0.78 (95% confidence interval 0.39-1.4), with 11 observed deaths versus 14 expected deaths.
“Very old patients treated with targeted agents have a comparable survival to an age- and sex-matched population, suggesting that initiating treatment in elderly and potentially frail patients is beneficial,” the authors concluded. “Dedicated studies are warranted for this clinical setting.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.