
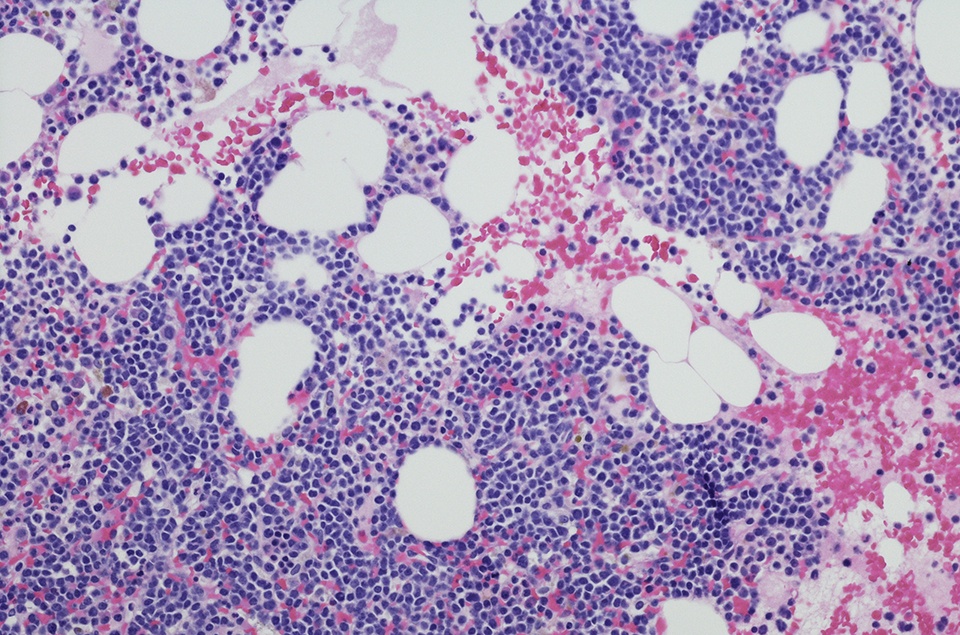
An analysis of real-world data regarding the treatment of patients with chronic lymphocytic leukemia revealed that standards of care are shifting from chemoimmunotherapy to targeted therapies. These findings were presented as a poster at the 2021 ASH Annual Meeting.
“As more therapies enter the clinic, real-world data are important to understand changes in the CLL treatment landscape and describe treatment patterns, to guide decisions on treatment strategies,” the authors wrote. In this retrospective analysis, the researchers searched a de-identified U.S. administrative claims database to identify patients diagnosed with CLL and treated with chemotherapy, CD20 monoclonal antibodies, Bruton tyrosine kinase (BTK) inhibitors, or B-cell lymphoma 2 (BCL2) inhibitors between 2016 and 2020. They also reviewed electronic health records from oncology practices to evaluate treatment patterns among adults diagnosed with CLL/small lymphocytic lymphoma and treated with BTK and/or BCL2 inhibitors.
In the claims database, annual treatment rate among patients diagnosed with CLL increased from 16% (n = 1,788/10,911) in 2016 to 26% (n = 2,441/9,349) in 2020. The proportion of patients treated with BTK inhibitors increased substantially (from 40% in 2016 to 65% in 2020), as did use of BCL2 inhibitors (from <1% to 13%). The authors observed corresponding decreases in the use of chemotherapies and CD20 monoclonal antibodies.
Two-thirds of the patients who initiated BTK inhibitors during the study period had previously untreated CLL, and the most common initial regimen was BTK inhibitor monotherapy (95%).
Few patients switched from BTK inhibitor monotherapy to CD20 monoclonal antibody (3%) or added CD20 monoclonal antibody to BTK inhibitor monotherapy (3%) within one year of treatment initiation, the authors added.
Among those who began BCL2 inhibitors, most patients had received prior treatment (85%), and the most common regimens were BCL2 inhibitor monotherapy (80%) or with CD20 monoclonal antibody (16%). However, a larger portion of patients who received initial BCL2 inhibitor monotherapy eventually added a CD20 monoclonal antibody within 12 months (30%). Treatment persistence at 12 months was similar for BTK and BCL2 inhibitors (63% and 61%, respectively).
In the electronic health records analysis, however, discontinuation rates were high for patients receiving BTK and BCL2 inhibitors (62% and 61%, respectively). Toxicity was the most common reason for discontinuation (54% for BTK and 36% for BCL2). Twelve percent of patients discontinued BTK inhibitors due to disease progression, while 30% of patients discontinued BCL2 inhibitors due to completion of regimen. The authors also found that the median treatment duration was comparable between monotherapy and combination regimens for both BTK (782 vs. 809 days) and BCL2 (747 vs. 718 days) inhibitors.
The authors also observed slow adoption of fixed-duration therapy with the BCL2 inhibitor combination regimen, while a high number of patients initiating combination regimens continued on monotherapy regimens, which contrasts with the regimens studied in randomized controlled trials.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.