
From the Chair
IgA nephropathy (IgAN) is the commonest primary glomerular disease globally.1 It can present quite benignly as microscopic hematuria with scattered mesangial deposits of IgA, as nephrotic syndrome, or in a more fulminant form as rapidly progressive glomerulonephritis with crescents on kidney biopsy. It affects children and adults, young and old. Some studies suggest that IgAN might be more common among Asian populations, but ascertainment bias for this observation has been suggested. Hitherto, the main approaches to therapy have centered around supportive measures such as renin angiotensin system (RAS) blockade and, more recently, sodium-glucose cotransporter-2 inhibitor therapy, both of which aim to slow kidney progression. In patients at high risk, including those with heavy proteinuria (>1 g/24 hours) or whose renal biopsy findings suggest a more aggressive course, therapy with corticosteroids and endothelin blockade (eg, sparsentan) has been recommended. Specific therapy targeted at the underlying etiology has proved elusive, at least so far.
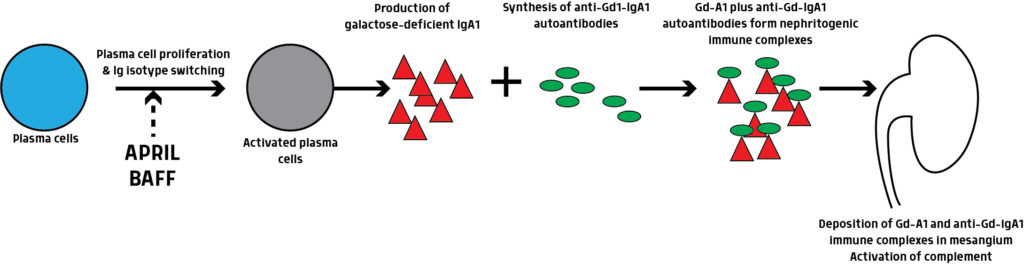
In 1993, Mestecky proposed that defective galactosylation and clearance of IgA1 molecules could be of etiopathogenic significance in IgAN.2 Subsequently, in 1999, Tomana, from Mestecky’s group, demonstrated that the circulating immune complexes in IgAN consist of IgA1 with galactose-deficient hinge region and published the results in the Journal of Clinical Investigation.3 That the central defect in IgAN is the production of IgA1 deficient in galactose residues in its hinge region was a pivotal discovery. It quickly became evident that galactose-deficient IgA1 (Gd-IgA1) stimulates the production of pathogenic or nephritogenic autoantibodies, which in turn lead to the production of circulating Gd-IgA1 immune complexes that deposit in the mesangium. However, because mesangial IgA deposition in and of itself does not cause disease, a multihit process has been proposed. Other hits are also thought to be very important: abnormal signaling in IgA1-producing cells; cytokines such as the TNF superfamily molecule, “a proliferation-inducing ligand,” or APRIL; activation of complement; and genetic factors, because increased levels of Gd-IgA1 is a hereditable trait.
The immunopathologic mechanisms underlying IgAN had been poorly understood, resulting in a lack of a specific therapy. The unraveling of the immunopathogenesis of IgA1 has resulted in many lines of investigation and drug development.4 Now, we are on the verge of having definitive targeted therapy available for IgAN.
APRIL has emerged as a critical factor in the pathogenesis of IgAN and is the focus of several clinical development programs. It has been implicated in two processes in IgAN (see Figure): mediating the Ig isotype switch during B-cell development that leads to production of IgA and galactose-deficient IgA1 and prolonging plasma cell survival.
Serum APRIL levels are elevated in patients with IgAN, and higher APRIL levels are associated with more rapidly progressive kidney disease. Visterra, which is now part of Otsuka, was the first major company to develop and publish its work on APRIL. Other companies are not far behind.
The Visterra molecule is sibeprenlimab, a humanized IgG2 monoclonal antibody that binds to and neutralizes APRIL. In first-to-human studies, sibeprenlimab demonstrated remarkable efficacy in reversibly reducing serum IgA and Gd-IgA1 in human volunteers.5 In a mouse model of IgAN (ddY mice), anti-APRIL antibodies reduced both IgA and Gd-IgA1 levels, reduced kidney-localized complement C3, and substantially reduced immune deposits in the kidney.6 In January 2024, the phase 2 ENVISION study of sibeprenlimab was published in the New England Journal of Medicine.7 In that study, Mathur and colleagues provided the first clinical glimpse of a therapy that specifically interfered with the immunopathogenesis of IgAN. Briefly, ENVISION was a double-blind, randomized, placebo-controlled, parallel group trial. Patients with IgAN at high risk of progression despite standard care for IgAN and maximized RAS blockade received 2, 4, or 8 mg/kg body weight or placebo monthly over 12 months. The primary end point was a surrogate outcome: change from baseline in the log-transformed 24-hour urinary protein to creatinine ratio (UPCR) at 12 months. Secondary end points included a change in estimated glomerular filtration rate (eGFR) at 12 months compared with baseline, changes in UPCR at 9 and 16 months compared with baseline, and changes in immunoglobulin levels of IgA, IgM, and IgG at various points.
ENVISION enrolled 155 patients. A total of 117 were randomized to one of three different monthly doses of sibeprenlimab, and 38 received placebo. At 12 months there was a dose-dependent 47% to 62% reduction in UPCR in patients who received sibeprenlimab (2-mg dosing was associated with a 47% reduction, 4 mg with 59%, and 8 mg with 62%, respectively, in UPCR). There also appeared to be a less steep decline in eGFR over 12 months in patients treated with sibeprenlimab as compared with placebo. Patients treated with higher doses of sibeprenlimab (4 mg and 8 mg) had an approximate 65% reduction in Gd-IgA1 and IgA, which then recovered to their baseline levels after discontinuation of sibeprenlimab. Treatment with the higher doses of sibeprenlimab led to a persistent reduction in proteinuria (even at 16 months, ie, several months after discontinuation of sibeprenlimab therapy). However, higher levels of sibeprenlimab (4 mg and 8 mg) were needed to persistently suppress APRIL and Gd-Ig-A1 antibody levels beyond 12 months.
Sibeprenlimab was well-tolerated, at least over the duration of the study. Adverse events in patients treated with sibeprenlimab were similar to those in the placebo group. There was no heightened risk of infection among sibeprenlimab patients compared with placebo.
What does this all mean? First, blocking APRIL with sibeprenlimab effectively inhibits the causal pathway to IgAN with no obvious adverse consequences. Second, and more broadly, designer-made antibodies like sibeprenlimab can target important mediators and could be applied to many other diseases—an obvious example being lupus nephritis. Third, targeting APRIL, which works by depleting B-cell activity but does so specifically, may allow future therapies to become more focused and therefore better tolerated.
The ENVISION study was only a phase 2 trial, and so additional work (eg, a phase 3 study) on a larger number of patients with longer follow-up and more hard end points is needed, although an interim approval based on the phase 2 data is possible.
Questions remain. It is unclear how long patients should be exposed to the therapy and what the longer-term side effects might be, but much progress has been made. We are now at the threshold of a new era.
Disclosure: Dr. Singh is chair of the Data Monitoring Committee for the BEYOND clinical trial (BION-1301) sponsored by Chinook.
References
- Rajasekaran A, Julian BA, Rizk DV. IgA nephropathy: an interesting autoimmune kidney disease. Am J Med Sci. 2021;361(2):176-194. doi:10.1016/j.amjms.2020.10.003
- Tomana M, Novak J, Julian BA, Matousovic K, Konecny K, Mestecky J. Circulating immune complexes in IgA nephropathy consist of IgA1 with galactose-
deficient hinge region and antiglycan antibodies. J Clin Invest. 1999;104(1):73-81. doi:10.1172/JCI5535 - Mestecky J, Tomana M, Crowley-Nowick PA, Moldoveanu Z, Julian BA, Jackson S. Defective galactosylation and clearance of IgA1 molecules as a possible etiopathogenic factor in IgA nephropathy. Contrib Nephrol. 1993;104:172-182. doi:10.1159/000422410
- Lim RS, Yeo SC, Barratt J, Rizk DV. An update on current therapeutic options in IgA nephropathy. J Clin Med. 2024;13(4):947. doi:10.3390/jcm13040947
- Mathur M, Barratt J, Suzuki Y, et al. Safety, tolerability, pharmacokinetics, and pharmacodynamics of VIS649 (sibeprenlimab), an APRIL-neutralizing IgG2
monoclonal antibody, in healthy volunteers. Kidney Int Rep. 2022;7(5):993-1003. doi:10.1016/j.ekir.2022.01.1073 - Myette JR, Kano T, Suzuki H, et al. A proliferation inducing ligand (APRIL) targeted antibody is a safe and effective treatment of murine IgA nephropathy. Kidney Int. 2019;96(1):104-116. doi:10.1016/j.kint.2019.01.031
- Mathur M, Barratt J, Chacko B, et al; ENVISION Trial Investigators Group. A phase 2 trial of sibeprenlimab in patients with IgA nephropathy. N Engl J Med. 2024;390(1):20-31. doi:10.1056/NEJMoa2305635





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.